ANZUPGO Cream Ref.[114507] Active ingredients: Delgocitinib
Source: European Medicines Agency (EU) Revision Year: 2024 Publisher: LEO Pharma A/S, Industriparken 55, DK-2750 Ballerup, Denmark
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Other dermatological preparations, agents for dermatitis, excluding corticosteroids
ATC code: D11AH11
Mechanism of action
Delgocitinib is a pan Janus kinase (JAK) inhibitor that targets the activity of all four members of the JAK family of enzymes consisting of JAK1, JAK2, JAK3, and tyrosine kinase 2 (TYK2) in a concentration dependent manner.
In human cells, inhibition of the JAK-STAT pathway by delgocitinib attenuates the signalling of several pro-inflammatory cytokines (including interleukin (IL)-2, IL-4, IL-6, IL-13, IL-21, IL-23, Granulocyte-Macrophage-Colony-Stimulating Factor (GM-CSF), and Interferon (IFN)-α) downregulating the immune and inflammatory responses in cells of relevance to CHE pathology.
Pharmacodynamic effects
In a thorough QT study in healthy subjects, there was no indication of a QTc prolonging effect of orally administered delgocitinib at single doses up to 12 mg (approximately 200 times the human 6 exposure following topical application, based on Cmax). Therefore, Anzupgo is not expected to affect cardiac repolarisation under conditions of clinical use.
Dermal safety studies
Clinical studies in healthy subjects demonstrated that delgocitinib cream did not cause phototoxic skin reactions or photoallergic skin reactions.
Clinical efficacy and safety
The safety and efficacy of delgocitinib cream were evaluated in two pivotal randomised, double-blind, vehicle-controlled studies of similar design (DELTA 1 and DELTA 2). CHE was defined as hand eczema that has persisted for more than 3 months or returned twice or more within the last 12 months. The studies included 960 patients 18 years of age and older with moderate to severe CHE as defined by an Investigator's Global Assessment for chronic hand eczema (IGA-CHE) score of 3 or 4 (moderate or severe) (see Table 2) and required a Hand Eczema Symptom Diary (HESD) itch score of ≥4 points at baseline. Eligible patients had a previous inadequate response to topical corticosteroids or were those in which topical corticosteroids are not advisable (e.g. due to important side effects or safety risks).
Table 2. Investigator's Global Assessment for chronic hand eczema (IGA-CHE):
| IGA-CHE severity | IGA-CHE score | Sign and intensity |
|---|---|---|
| Clear | 0 | No signs of erythema, scaling, hyperkeratosis/lichenification, vesiculation, oedema or fissures |
| Almost clear | 1 | Barely perceptible erythema No signs of scaling, hyperkeratosis/lichenification, vesiculation, oedema or fissures |
| Mild | 2 | At least one: • Slight but definite erythema (pink) • Slight but definite scaling (mostly fine scales) • Slight but definite hyperkeratosis/lichenification and at least one: • Scattered vesicles, without erosion • Barely palpable oedema • Superficial fissures |
| Moderate | 3 | At least one: • Clearly perceptible erythema (dull red) • Clearly perceptible scaling (coarse scales) • Clearly perceptible hyperkeratosis/lichenification and at least one: • Clustered vesicles, without visible erosions • Definite oedema • Definite fissures |
| Severe | 4 | At least one: • Marked erythema (deep or bright red) • Marked and thick scaling • Marked hyperkeratosis/lichenification and at least one: • High density of vesicles with erosions • Marked oedema • One or more deep fissures |
In DELTA 1 and DELTA 2, patients applied either delgocitinib 20 mg/g cream or vehicle cream twice daily to affected areas on the hands and wrists for 16 weeks. All patients who completed the two pivotal studies were eligible to enrol into the long-term extension study DELTA 3.
Endpoints
In DELTA 1 and DELTA 2, the primary endpoint was the proportion of patients achieving IGA-CHE treatment success (IGA-CHE TS), defined as an IGA-CHE score of 0 (clear) or 1 (almost clear: barely perceptible erythema only) with at least a 2-step improvement from baseline to Week 16. The IGA-CHE instrument rates the severity of the subject's global disease and is based on a 5-point scale ranging from 0 (clear) to 4 (severe).
Additional efficacy outcomes included the Hand Eczema Severity Index (HECSI) and the HESD at various timepoints. The HECSI rates the severity of six clinical signs (erythema, infiltration/papulation, vesicles, fissures, scaling, and oedema) and the extent of the lesions on each of the five hand regions (fingertips, fingers, palm of hands, back of hands, and wrists). The HESD is a daily 6-item patient-reported outcome (PRO) instrument designed to assess the worst severity of signs and symptoms of CHE (itch, pain, cracking, redness, dryness, and flaking) using an 11-point numeric rating scale.
Baseline characteristics
Across all treatment groups in DELTA 1 and DELTA 2, the mean age was 44.1 years, 7.6% of patients were 65 years of age or older, 64.4% were female, 90.4% were White, 3.5% were Asian, and 0.7% were Black. The frequency of CHE by main subtype was 35.9% atopic hand eczema, 21.5% hyperkeratotic eczema, 19.6% irritant contact dermatitis, 13.9% allergic contact dermatitis, 9.1% vesicular hand eczema (pompholyx), and 0.1% contact urticaria/protein contact dermatitis. In DELTA 1 and DELTA 2, 71.6% of patients had a baseline IGA-CHE score of 3 (moderate CHE), and 28.4% of patients had a baseline IGA-CHE score of 4 (severe CHE). The mean baseline Dermatology Life Quality Index (DLQI) score was 12.5, HECSI score was 71.6, and HESD score was 7.1. The mean HESD itch and pain scores were 7.1 and 6.7, respectively.
Clinical response
DELTA 1 and DELTA 2
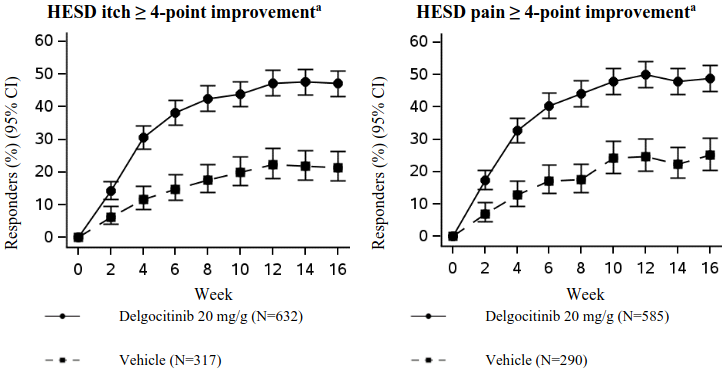
In DELTA 1 and DELTA 2, a statistically significantly greater proportion of patients randomised to delgocitinib cream achieved the primary endpoint of IGA-CHE TS compared to vehicle at Week 16. The results for the primary and most relevant multiplicity-controlled secondary endpoints are presented in Table 3. Figure 1 shows the proportion of patients who achieved HESD itch ≥4-point improvement, and HESD pain ≥4-point improvement over time in DELTA 1 and DELTA 2.
Table 3. Efficacy results of delgocitinib at Week 16 in DELTA 1 and DELTA 2:
| DELTA 1 | DELTA 2 | |||
|---|---|---|---|---|
| Delgocitinib (N=325) | Vehicle (N=162) | Delgocitinib (N=313) | Vehicle (N=159) | |
| IGA-CHE TS, % respondersa | 19.7# | 9.9 | 29.1§ | 6.9 |
| HECSI-90, % respondersa,b | 29.5§ | 12.3 | 31.0§ | 8.8 |
| HECSI-75, % respondersa,c | 49.2§ | 23.5 | 49.5§ | 18.2 |
| HECSI, LS mean % change from baseline (± SE)d | -56.5§ (± 3.4) | -21.2 (± 4.8) | -58.9§ (± 3.2) | -13.4 (± 4.5) |
| HESD itch ≥4-point improvement, % respondersa,e | 47.1§ (152/323) | 23.0 (37/161) | 47.2§ (146/309) | 19.9 (31/156) |
| HESD pain ≥4-point improvement, % respondersa,e | 49.1§ (143/291) | 27.5 (41/149) | 48.6§ (143/294) | 22.7 (32/141) |
| HESD ≥4-point improvement, % respondersa,e | 47.2§ (146/309) | 24.4 (38/156) | 44.5§ (137/308) | 20.9 (32/153) |
# p<0.01, §p<0.001
All p-values were statistically significant versus vehicle with adjustment for multiplicity.
Abbreviations: LS=least squares; N=number of patients in the full analysis set (all patients randomised and dosed); SE=standard error
a Data after initiation of rescue treatment, permanent discontinuation of treatment, or missing data were considered non-response.
b HECSI-90 responders were patients with ≥90% improvement in HECSI from baseline.
c HECSI-75 responders were patients with ≥75% improvement in HECSI from baseline.
d Data after initiation of rescue treatment, permanent discontinuation of treatment, or missing data were considered non-response by using worst observation carried forward.
e Based on the number of patients whose baseline value was ≥4 (scale from 0-10).
In both DELTA 1 and DELTA 2, a statistically significantly greater proportion of patients treated with delgocitinib cream achieved IGA-CHE TS and a ≥4-point improvement in HESD as early as Week 4 compared to vehicle. A statistically significantly greater proportion of patients treated with delgocitinib cream achieved HECSI-75 at Week 8 compared to vehicle.
Figure 1. Proportion of patients who achieved HESD itch ≥4-point improvement and HESD pain ≥4-point improvement over time – pooled data from DELTA 1 and DELTA 2:
CI = Confidence Interval
a Based on the number of patients whose baseline value was ≥4 (scale from 0-10).
Additional quality of life/patient-reported outcomes
In both DELTA 1 and DELTA 2, patients treated with delgocitinib cream showed a statistically significantly greater improvement from baseline to Week 16 compared to vehicle in the Hand Eczema Impact Scale (HEIS) (see Table 4). HEIS is an instrument used for assessing the patient's perceived impact on their daily activities (use of soaps/cleaning products, housework involving hands getting wet, washing themselves, embarrassment, frustration, sleep, work, and the ability to hold or grip objects). 9 items are scored on a 5-point scale where 0='not at all' and 4='extremely', and the HEIS score is then calculated as the average of the 9 items.
Across DELTA 1 and DELTA 2, statistically significantly greater improvements in health-related quality of life, as measured by the DLQI were observed in delgocitinib patients compared to vehicle at Week 16 (see Table 4).
Table 4. Quality of life/patient-reported outcomes results of delgocitinib at Week 16 in DELTA 1 and DELTA 2:
| DELTA 1 | DELTA 2 | |||
|---|---|---|---|---|
| Delgocitinib (N=325) | Vehicle (N=162) | Delgocitinib (N=313) | Vehicle (N=159) | |
| HEIS, LS mean change from baseline (± SE)a | -1.46§ (± 0.05) | -0.82 (± 0.08) | -1.45§ (± 0.06) | -0.64 (± 0.08) |
| HEIS PDAL, LS mean change from baseline (± SE)a,b | -1.46§ (± 0.06) | -0.86 (± 0.08) | -1.48§ (± 0.06) | -0.66 (± 0.08) |
| DLQI ≥4-point improvement, % respondersc,d | 74.4§ (227/305) | 50.0 (74/148) | 72.2§ (216/299) | 45.8 (70/153) |
§ p<0.001
All p-values were statistically significant versus vehicle with adjustment for multiplicity.
Abbreviations: LS=least squares; N=number of patients in the full analysis set (all patients randomised and dosed); PDAL=proximal daily activity limitations; SE=standard error
a Data after initiation of rescue treatment, permanent discontinuation of treatment, or missing data were considered non-response by using worst observation carried forward.
b HEIS PDAL assesses the patient's ability to use soaps/cleaning products, to do housework, and to wash themselves. The HEIS PDAL score is calculated as the average of the 3 items.
c Data after initiation of rescue treatment, permanent discontinuation of treatment, or missing data were considered non-response.
d Based on the number of patients whose baseline value was ≥4.
Extension study (DELTA 3)
Patients who completed either DELTA 1 or DELTA 2 were eligible to enrol in a 36-week open-label extension study (DELTA 3). In DELTA 3, the long-term safety and efficacy of as-needed delgocitinib treatment was evaluated in 801 patients. Patients started application of delgocitinib cream twice daily to affected areas whenever the IGA-CHE score was ≥2 (mild or worse) and stopped treatment when an IGA-CHE score of 0 or 1 (clear or almost clear) was achieved. Patients entering DELTA 3 with an IGA-CHE score of 0 or 1 remained off treatment until loss of response (IGA-CHE score ≥2).
The proportions of patients achieving IGA-CHE 0 or 1, HECSI-75, HECSI-90, HESD itch ≥4-point improvement, and HESD pain ≥4-point improvement after the initial 16-week treatment period of delgocitinib cream were maintained through Week 52 with as-needed treatment. Among the 560 patients randomised to delgocitinib cream treatment in the pivotal studies (DELTA 1 and DELTA 2) enrolled in DELTA 3, the mean number of treatment periods was 1.5 (range 0 to 6), the mean treatment period duration was 123 days, and the mean cumulative number of days in response (days with an IGA-CHE score of 0 or 1 within the 36-week treatment period) was 46. The mean cumulative number of days in response was 111 among those patients who achieved IGA-CHE TS at Week 16 in the pivotal studies.
Of the patients randomised to delgocitinib cream in the pivotal studies who achieved IGA-CHE TS at Week 16, the median duration of response while off treatment was 4 weeks with 28.3% maintaining response for at least 8 weeks. The median time to regain an IGA-CHE score of 0 or 1 following re-initiation of treatment was 8 weeks. Among patients who did not achieve an IGA-CHE TS at Week 16 of delgocitinib treatment in the pivotal studies, 48.1% achieved IGA-CHE 0 or 1 with continued delgocitinib treatment in DELTA 3.
Paediatric population
The European Medicines Agency has deferred the obligation to submit the results of studies with delgocitinib in one or more subset of the paediatric population for the treatment of chronic hand eczema (see section 4.2 for information on paediatric use).
5.2. Pharmacokinetic properties
Absorption
The pharmacokinetics of delgocitinib cream were evaluated in a study involving 15 adult patients 22 to 69 years of age with moderate to severe CHE. Patients applied on average 0.87 g of delgocitinib 20 mg/g cream to the affected areas of the hands and wrists twice a day for 8 days.
The geometric mean (GSD) maximum plasma concentration (Cmax) and area under the concentration-curve from time 0 to 12 hours (AUC0-12) on Day 8 was 0.46 ng/mL (1.74) and 3.7 ng*h/mL (1.74), respectively. Steady state was reached by Day 8. The systemic exposure (AUC and Cmax) between Day 1 and Day 8 were similar.
Following twice daily application of delgocitinib 20 mg/g cream in DELTA 2, the geometric mean plasma concentration observed 2-6 hours after application at Day 113 was 48% lower than that at Day 8 (0.11 ng/mL and 0.21 ng/mL, respectively).
The relative bioavailability of delgocitinib following topical application is approximately 0.6% compared to administration via oral tablets.
Distribution
Based on an in vitro study, plasma protein binding of delgocitinib is 22 to 29%.
Biotransformation
As delgocitinib does not undergo extensive metabolism, the main plasma component is unchanged delgocitinib. Following oral administration, four metabolites (formed via oxidation and glucuronide conjugation) were detected at <2% of the average unchanged delgocitinib plasma concentrations. The limited metabolism of delgocitinib occurs primarily though CYP3A4/5 and to a lesser extent by CYP1A1, CYP2C19, and CYP2D6.
In vitro interaction studies
Based on in vitro data, delgocitinib does not inhibit or induce cytochrome P450 enzymes or inhibit transporter systems such as organic anion transporters (OAT), organic anion transporting polypeptides (OATP), organic cation transporters (OCT), P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), or multidrug and toxin extrusion proteins (MATE) at clinically relevant concentrations.
Delgocitinib is a substrate of P-glycoprotein (P-gp) and a weak substrate of human organic cation transporter 2 (OTC2) and human organic anion transporter 3 (OAT3).
Elimination
Delgocitinib is primarily eliminated by renal excretion as approximately 70-80% of the total dose after oral administration was found unchanged in the urine.
Following repeated topical application of delgocitinib cream, the average half-life of delgocitinib was estimated to be 20.3 hours.
Special populations
Hepatic impairment
No formal studies of delgocitinib cream in patients with hepatic impairment have been conducted.
Due to the minimal systemic exposure of topically applied delgocitinib and limited metabolism of delgocitinib, changes in hepatic function are unlikely to have any effect on the elimination of delgocitinib (see section 4.2).
Renal impairment
Pharmacokinetic parameters of delgocitinib were analysed in 96 patients with mild or moderate renal impairment (eGFR 30 to 89 mL/min/1.73 m²) in DELTA 2. There were no clinically relevant differences in the pharmacokinetics observed in patients with mild or moderate renal impairment compared to the overall study population. Renal function impairment is unlikely to result in clinically important changes in exposure to delgocitinib due to the minimal systemic exposure following topical administration (see section 4.2).
5.3. Preclinical safety data
Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, genotoxicity, phototoxicity, local tolerability, skin sensitisation, and juvenile toxicity. Effects in repeat dose toxicity studies were observed only at exposures considered sufficiently in excess of the maximum human exposure following topical application.
Carcinogenicity
In a 2-year dermal carcinogenicity study in mice, no local or systemic drug-related neoplastic findings were observed (at exposures up to approximately 600 times the human exposure based on AUC).
Fertility and early embryonic development
Orally administered delgocitinib did not result in effects on fertility at any dose level evaluated in male rats (exposures approximately 1 700 times the human exposure). In female rats, orally administered delgocitinib resulted in effects on female fertility (lower fertility index, fewer corpora lutea, and fewer implantations) at exposures approximately 5 800 times the human exposure. Post-implantation losses and a decrease in the number of live embryos were observed at exposures approximately 432 and 1 000 times the human exposure, respectively.
Embryo-foetal development
Orally administered delgocitinib did not result in adverse effects to the foetus in rats or rabbits at exposures approximately 120 and 194 times the human exposure, respectively. Teratogenic effects were not observed at any dose studied in rats or rabbits (exposures approximately 1 400 and 992 times the human exposure, respectively).
In rats, decreases in foetal weight and skeletal variations were observed at exposures 512 times the human exposure and a tendency toward an increase in post-implantation loss was observed at exposures approximately 1 400 times the human exposure. In rabbits, an increase in post-implantation 12 loss, a reduced number of live foetuses, and a tendency toward a decrease in foetal weights were observed at exposures approximately 992 times the human exposure.
No effects during pregnancy are anticipated, since systemic exposure to delgocitinib is negligible. As a precautionary measure, it is preferable to avoid the use of delgocitinib during pregnancy (see section 4.6).
Pre-and postnatal development
Orally administered delgocitinib in rats resulted in decreased foetal viability and reduced pup weights during the early postnatal period at exposures > 2 000 times the human exposure. There was no effect on behavioural and learning assessments, sexual maturation, or reproductive performance of the offspring at any dose studied.
Following oral administration to lactating rats, delgocitinib was secreted in milk at concentrations approximately 3-fold those in the plasma.
No effects on the breastfed newborn/infant are anticipated since the systemic exposure in the breast-feeding woman to delgocitinib is negligible. Delgocitinib can therefore be used during breast-feeding (see section 4.6).
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.