ASPAVELI Solution for infusion Ref.[49950] Active ingredients: Pegcetacoplan
Source: European Medicines Agency (EU) Revision Year: 2024 Publisher: Swedish Orphan Biovitrum AB (publ), SE-112 76 Stockholm, Sweden
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Immunosuppressants, Selective immunosuppressants
ATC code: L04AA54
Mechanism of action
Pegcetacoplan is a symmetrical molecule comprised of two identical pentadecapeptides covalently bound to the ends of a linear 40-kDa PEG molecule. The peptide moieties bind to complement C3 and exert a broad inhibition of the complement cascade. The 40-kDa PEG moiety imparts improved solubility and longer residence time in the body after administration of the medicinal product.
Pegcetacoplan binds to complement protein C3 and its activation fragment C3b with high affinity, thereby regulating the cleavage of C3 and the generation of downstream effectors of complement activation. In PNH, extravascular haemolysis (EVH) is facilitated by C3b opsonisation while intravascular haemolysis (IVH) is mediated by the downstream membrane attack complex (MAC). Pegcetacoplan exerts broad regulation of the complement cascade by acting proximal to both C3b and MAC formation, thereby controlling the mechanisms that lead to EVH and IVH.
Pharmacodynamic effects
In Study APL2-302, the mean C3 concentration increased from 0.94 g/L at baseline to 3.83 g/L at Week 16 in the pegcetacoplan group and sustained through Week 48. In Study APL2-308, the mean C3 concentration increased from 0.95 g/L at baseline to 3.56 g/L at Week 26.
In Study APL2-302, the mean percentage of PNH Type II + III RBCs increased from 66.80% at baseline, to 93.85% at Week 16 and sustained through Week 48. In Study APL2-308, the mean percentage of PNH Type II + III RBCs increased from 42.4% at baseline to 90.0% at Week 26.
In Study APL2-302, the mean percentage of PNH Type II + III RBCs with C3 deposition was decreased from 17.73% at baseline to 0.20% at Week 16 and sustained through Week 48. In Study APL2-308, the mean percentage of PNH Type II + III RBCs with C3 deposition decreased from 2.85% at baseline to 0.09% at Week 26.
Clinical efficacy and safety
The efficacy and safety of pegcetacoplan in patients with PNH was assessed in two open-label, randomised-controlled phase 3 studies: in complement inhibitor-experienced patients in Study APL2-302 and in complement inhibitor-naïve patients in Study APL2-308. In both studies the dose of pegcetacoplan was 1 080 mg twice weekly. If required, the dose could be adjusted to 1 080 mg every 3 days.
Study in complement inhibitor-experienced adult patients (APL2-302)
Study APL2-302 was an open-label, randomised study with an active comparator-controlled period of 16 weeks followed by a 32-week open label period (OLP). This study enrolled patients with PNH who had been treated with a stable dose of eculizumab for at least the previous 3 months and with haemoglobin levels <10.5 g/dL. Eligible patients entered a 4-week run-in period during which they received pegcetacoplan 1 080 mg subcutaneously twice weekly in addition to their current dose of eculizumab. Patients were then randomised in a 1:1 ratio to receive either 1 080 mg of pegcetacoplan twice weekly or their current dose of eculizumab through the duration of the 16-week randomised controlled period (RCP). Randomisation was stratified based on the number of packed red blood cell (PRBC) transfusions within the 12 months prior to Day -28 (<4; ≥4) and platelet count at screening (<100 000/mm³; ≥100 000/mm³). Patients who completed the RCP entered the OLP during which all patients received pegcetacoplan for up to 32 weeks (patients who received eculizumab during the RCP entered a 4-week run-in period before switching to pegcetacoplan monotherapy).
The primary and secondary efficacy endpoints were assessed at Week 16. The primary efficacy endpoint was change from baseline to Week 16 (during RCP) in haemoglobin level. Baseline was defined as the average of measurements prior to the first dose of pegcetacoplan (at the beginning of the run-in period). Key secondary efficacy endpoints were transfusion avoidance, defined as the proportion of patients who did not require a transfusion during the RCP, and change from baseline to Week 16 in absolute reticulocyte count (ARC), LDH level, and FACIT-Fatigue scale score.
A total of 80 patients entered the run-in period. At the end of the run-in period, all 80 were randomised, 41 to pegcetacoplan and 39 to eculizumab. Demographics and baseline disease characteristics were generally well balanced between treatment groups (see Table 2). A total of 38 patients in the group treated with pegcetacoplan and 39 patients in the eculizumab group completed the 16-week RCP and continued into the 32-week open-label period. In total, 12 of 80 (15%) patients receiving pegcetacoplan discontinued due to adverse events. Per protocol 15 patients had their dose adjusted to 1 080 mg every 3 days. Twelve patients were evaluated for benefit and 8 of the 12 patients demonstrated benefit from the dose adjustment.
Table 2. Patient baseline demographics and characteristics in Study APL2-302:
| Parameter | Statistics | Pegcetacoplan (N=41) | Eculizumab (N=39) |
|---|---|---|---|
| Age (years) 18-64 years ≥65 years | Mean (SD) n (%) n (%) | 50.2 (16.3) 31 (75.6) 10 (24.4) | 47.3 (15.8) 32 (82.1) 7 (17.9) |
| Dose level of eculizumab at baseline Every 2 weeks IV 900 mg Every 11 days IV 900 mg Every 2 weeks IV 1 200 mg Every 2 weeks IV 1 500 mg | n (%) n (%) n (%) n (%) | 26 (63.4) 1 (2.4) 12 (29.3) 2 (4.9) | 29 (74.4) 1 (2.6) 9 (23.1) 0 |
| Female | n (%) | 27 (65.9) | 22 (56.4) |
| Time since diagnosis of PNH (years) to Day -28 | Mean (SD) | 8.7 (7.4) | 11.4 (9.7) |
| Haemoglobin level (g/dL) | Mean (SD) | 8.7 (1.1) | 8.7 (0.9) |
| Reticulocyte count (109/L) | Mean (SD) | 218 (75.0) | 216 (69.1) |
| LDH level (U/L) | Mean (SD) | 257.5 (97.6) | 308.6 (284.8) |
| Total FACIT-Fatigue* | Mean (SD) | 32.2 (11.4) | 31.6 (12.5) |
| Number of transfusions in last 12 months prior to Day -28 | Mean (SD) | 6.1 (7.3) | 6.9 (7.7) |
| <4 | n (%) | 20 (48.8) | 16 (41.0) |
| ≥4 | n (%) | 21 (51.2) | 23 (59.0) |
| Platelet count at screening (109/L) | Mean (SD) | 167 (98.3) | 147 (68.8) |
| Platelet count at screening <100 000/mm³ | n (%) | 12 (29.3) | 9 (23.1) |
| Platelet count at screening ≥100 000/mm³ | n (%) | 29 (70.7) | 30 (76.9) |
| History of aplastic anaemia | n (%) | 11 (26.8) | 9 (23.1) |
| History of myelodysplastic syndrome | n (%) | 1 (2.4) | 2 (5.1) |
* FACIT-Fatigue is measured on a scale of 0-52, with higher values indicating less fatigue.
Pegcetacoplan was superior to eculizumab for the primary endpoint of the haemoglobin change from baseline (P<0.0001).
Figure 1. Adjusted mean change in haemoglobin (g/dL) from baseline to Week 16 in APL2-302:
Non-inferiority was demonstrated in key secondary endpoints of transfusion avoidance and change from baseline in ARC.
Non-inferiority was not met in change from baseline in LDH.
Due to hierarchical testing, statistical testing for change from baseline for FACIT-Fatigue score was not formally tested.
The adjusted means, treatment difference, confidence intervals, and statistical analyses performed for the key secondary endpoints are shown in Figure 2.
Figure 2. Key secondary endpoints analysis in APL2-302:
Results were consistent across all supportive analyses of the primary and key secondary endpoints, including all observed data with post transfusion data included.
Haemoglobin normalisation was achieved in 34% of patients in the pegcetacoplan group versus 0% in the eculizumab group at Week 16. LDH normalisation was achieved in 71% of patients in the group treated with pegcetacoplan versus 15% in the eculizumab group.
A total of 77 patients entered the 32-week OLP, during which all patients received pegcetacoplan, resulting in a total exposure of up to 48 weeks. The results at Week 48 were generally consistent with those at Week 16 and support sustained efficacy.
Study in complement inhibitor-naïve adult patients (APL2-308)
Study APL2-308 was an open-label, randomised, controlled study that enrolled patients with PNH who had not been treated with any complement inhibitor within 3 months prior to enrolment and with haemoglobin levels less than the lower limit of normal (LLN). Eligible patients were randomised in a 2:1 ratio to receive pegcetacoplan or supportive care (e.g., transfusions, corticosteroids, supplements such as iron, folate, and vitamin B12), hereafter referred to as the control arm through the duration of the 26-week treatment period.
Randomisation was stratified based on the number of packed red blood cell (PRBC) transfusions within the 12 months prior to Day -28 (<4; ≥4). At any point during the study, a patient assigned to the control arm who had haemoglobin levels ≥2 g/dL below baseline or presented with a PNH associated thromboembolic event was per protocol able to transition to pegcetacoplan for the remainder of the study.
A total of 53 patients were randomised, 35 to pegcetacoplan and 18 patients to the control arm. Demographics and baseline disease characteristics were generally well balanced between treatment arms. The mean age was 42.2 years in the pegcetacoplan arm and 49.1 years in the control arm. The mean number of PRBC transfusions in the 12 months prior to screening was 3.9 in the pegcetacoplan arm and 5.1 in the control arm. Five patients in each arm (14.3% in the pegcetacoplan arm and 27.8% in the control arm) had a history of aplastic anaemia. Further baseline values were as follows: mean baseline haemoglobin levels (pegcetacoplan arm: 9.4 g/dL vs. control arm; 8.7 g/dL), ARC (pegcetacoplan arm: 230.2 × 109/L vs. control arm: 180.3 × 109/L), LDH (pegcetacoplan arm: 2 151.0 U/L vs. control arm: 1 945.9 U/L) and platelet count (pegcetacoplan arm: 191.4 × 109/L vs. control arm: 125.5 × 109/L). Eleven of 18 patients randomised to the control arm transitioned to pegcetacoplan because their haemoglobin levels decreased by ≥2 g/dL below baseline. Of the 53 randomised patients, 52 (97.8%) received prophylactic antibiotic therapy according to local prescribing guidelines.
The primary and secondary efficacy endpoints were assessed at Week 26. The two co-primary efficacy endpoints were haemoglobin stabilisation, defined as avoidance of a >1 g/dL decrease in haemoglobin concentration from baseline in the absence of transfusion, and change in LDH concentration from baseline.
In the group treated with pegcetacoplan, 30 out of 35 patients (85.7%) achieved haemoglobin stabilisation versus 0 patients in the control arm. The adjusted difference between pegcetacoplan and the control arm was 73.1% (95% CI, 57.2% to 89.0%; p<0.0001).
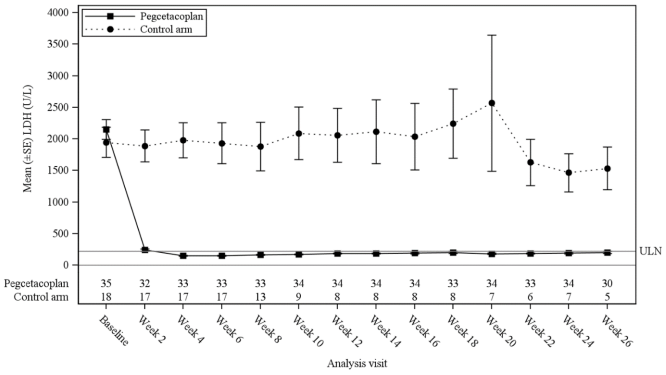
The least-square (LS) mean (SE) changes from baseline in LDH concentration at Week 26 were -1 870 U/L in the group treated with pegcetacoplan versus -400 U/L in the control arm (p<0.0001). The difference between pegcetacoplan and the control arm was -1 470 (95% CI, -2 113 to -827). Treatment differences between the pegcetacoplan and the control arm were evident at Week 2 and were maintained through Week 26 (Figure 3). LDH concentrations in the control arm remained elevated.
Figure 3. Mean (±SE) LDH concentration (U/L) over time by treatment group in study APL2-308:
For the selected key secondary efficacy endpoints of haemoglobin response in the absence of transfusions, change in haemoglobin level, and change in ARC, the group treated with pegcetacoplan demonstrated a significant treatment difference versus the control arm (Table 3).
Table 3. Key secondary endpoints analysis in study APL2-308:
| Parameter | Pegcetacoplan (N=35) | Control arm (N=18) | Difference (95% CI) p-value |
|---|---|---|---|
| Haemoglobin response in the absence of transfusionsa n (%) | 25 (71%) | 1 (6%) | 54% (34%, 74%) p<0.0001 |
| Change from baseline to Week 26 in haemoglobin level (g/dL) LS Mean (SE) | 2.9 (0.38) | 0.3 (0.76) | 2.7 (1.0, 4.4) |
| Change from baseline to Week 26 in ARC (109/L) LS Mean (SE) | -123 (9.2) | -19 (25.2) | -104 (-159, -49) |
a Haemoglobin response was defined as a ≥1 g/dL increase in haemoglobin from baseline at Week 26.
ARC = Absolute reticulocyte count, CI = Confidence interval, LS = Least square, SE = Standard error
Paediatric population
The European Medicines Agency has deferred the obligation to submit the results of studies with ASPAVELI in one or more subsets of the paediatric population in paroxysmal nocturnal haemoglobinuria (see section 4.2 for information on paediatric use).
5.2. Pharmacokinetic properties
Absorption
Pegcetacoplan is administered by subcutaneous infusion and gradually absorbed into the systemic circulation with a median Tmax between 108 and 144 hours (4.5 to 6.0 days) following a single subcutaneous dose to healthy volunteers. Steady-state serum concentrations following twice weekly dosing at 1 080 mg in patients with PNH were achieved approximately 4 to 6 weeks following the first dose. In complement inhibitor-experienced patients (Study APL2-302) the geometric mean (CV) steady-state serum concentrations ranged between 655 (18.6) and 706 (15.1%) µg/mL in patients treated for 16 weeks. Steady-state concentrations in the patients (n=22) that continued to receive pegcetacoplan up to Week 48 were 623 µg/mL (39.7%), indicating sustainable therapeutic concentrations of pegcetacoplan through Week 48. In complement inhibitor-naïve patients (Study APL2-308) the geometric mean (CV) steady-state serum concentration at Week 26 was 744 µg/mL (25.5) with twice weekly dosing. The bioavailability of a subcutaneous dose of pegcetacoplan is estimated to be 76% based on population PK analysis.
Distribution
The mean (CV) volume of distribution of pegcetacoplan is approximately 3.98 L (32) in patients with PNH based on population PK analysis.
Metabolism/elimination
Based on its PEGylated peptide structure, the metabolism of pegcetacoplan is expected to occur via catabolic pathways and be degraded into small peptides, amino acids, and PEG. Results of a radiolabelled study in cynomolgus monkeys suggest the primary route of elimination of the labelled peptide moiety is via urinary excretion. Although the elimination of PEG was not studied, it is known to undergo renal excretion.
Pegcetacoplan showed no inhibition or induction of the CYP enzyme isoforms tested as demonstrated from the results of in vitro studies. Pegcetacoplan was neither a substrate nor an inhibitor of the human uptake or efflux transporters.
Following multiple subcutaneous dosing of pegcetacoplan in patients with PNH, the mean (CV) clearance is 0.015 L/h (30) and median effective half-life of elimination (t1/2) is 8.6 days as estimated by the population PK analysis.
Linearity/non-linearity
Exposure of pegcetacoplan increases in a dose proportional manner from 45 to 1 440 mg.
Special populations
No impact on the pharmacokinetics of pegcetacoplan was identified with age (19-81 years), race or sex based on the results of population PK analysis.
Compared with a reference 70 kg patient, the steady-state average concentration is predicted to be approximately 20% higher in patients with a body weight of 50 kg. Patients weighing 40 kg are predicted to have a 45% higher average concentration. Minimal data are available on the safety profile of pegcetacoplan for patients with a body weight below 50 kg.
Elderly
Although there were no apparent age-related differences observed in these studies, the number of patients aged 65 years and over is not sufficient to determine whether they respond differently from younger patients. See section 4.2.
Renal impairment
In a study of 8 patients with severe renal impairment, defined as creatinine clearance (CrCl) less than 30 mL/min using the Cockcroft-Gault formula (with 4 patients with values less than 20 mL/min), renal impairment had no effect on the pharmacokinetics of a single 270-mg dose of pegcetacoplan. There are minimal data on patients with PNH with renal impairment who have been administered the clinical dose of 1 080 mg twice weekly. There are no available clinical data for the use of pegcetacoplan in patients with ESRD requiring haemodialysis. See section 4.2.
5.3. Preclinical safety data
In vitro and in vivo toxicology data reveal no toxicity of special concern for humans. Effects observed in animals at exposure levels similar to clinical exposure levels are described below. These effects were not observed in clinical studies.
Animal reproduction
Pegcetacoplan treatment of pregnant cynomolgus monkeys at a subcutaneous dose of 28 mg/kg/day (2.9 times the human steady-state Cmax) from the gestation period through parturition resulted in a statistically significant increase in abortions or stillbirths. No maternal toxicity or teratogenic effects were observed in offspring delivered at term. Additionally, no developmental effects were observed in infants up to 6 months postpartum. Systemic exposure to pegcetacoplan was detected in foetuses from monkeys treated with 28 mg/kg/day from the period of organogenesis through the second trimester, but the exposure was minimal (less than 1%, not pharmacologically significant).
Carcinogenesis
Long term animal carcinogenicity studies of pegcetacoplan have not been conducted.
Genotoxicity
Pegcetacoplan was not mutagenic when tested in in vitro bacterial reverse mutation (Ames) assays and was not genotoxic in an in vitro assay in human TK6 cells or in an in vivo micronucleus assay in mice.
Animal toxicology
Repeat-dose studies were conducted in rabbits and cynomolgus monkeys with daily subcutaneous doses of pegcetacoplan up to 7 times the human dose (1 080 mg twice weekly). Histologic findings in both species included dose-dependent epithelial vacuolation and infiltrates of vacuolated macrophages in multiple tissues. These findings have been associated with large cumulative doses of long-chain PEG in other marketed PEGylated drugs, were without clinical consequence, and were not considered adverse. Reversibility was not demonstrated in the pegcetacoplan animal studies after one month and was not evaluated for a longer duration. Data from literature suggest reversibility of PEG vacuoles.
Renal tubular degeneration was observed microscopically in both species at exposures (Cmax and AUC) less than or comparable to those for the human dose and was minimal and nonprogressive between 4 weeks and 9 months of daily administration of pegcetacoplan. Although no overt signs of renal dysfunction were observed in animals, the clinical significance and functional consequence of these findings are unknown.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.