COAGADEX Powder and solvent for solution for injection Ref.[9429] Active ingredients: Coagulation factor X
Source: European Medicines Agency (EU) Revision Year: 2020 Publisher: BPL Bioproducts Laboratory GmbH, Dornhofstraße 34, 63263, Neu-Isenburg, Germany
Therapeutic indications
Coagadex is indicated for the treatment and prophylaxis of bleeding episodes and for perioperative management in patients with hereditary factor X deficiency.
Coagadex is indicated in all age groups.
Posology and method of administration
Treatment should be initiated under the supervision of a physician experienced in the treatment of rare bleeding disorders.
Posology
The dose and duration of the treatment depend on the severity of the factor X deficiency (i.e. the patient's baseline factor X level), on the location and extent of the bleeding and on the patient's clinical condition.
Careful control of replacement therapy is especially important in cases of major surgery or life-threatening bleeding episodes.
Not more than 60 IU/kg daily should be administered in any age group.
In adults and adolescents at least 12 years of age, the expected in vivo peak increase in factor X level expressed as IU/dL (or % of normal) can be estimated using the following formulae:
Dose (IU) = body weight (kg) x desired factor X rise (IU/dL or % of normal) x 0.5
OR
Increase in factor X level (IU/dL or % of normal) = [total dose (IU)/body weight (kg)] x 2
The following examples assume the patient's baseline factor X level is <1 IU/dL:
- A dose of 2000 IU Coagadex administered to a 70 kg patient should be expected to result in a peak post-infusion factor X increase of 2000 x {[2 IU/dL]/[IU/kg]}/[70 kg] = 57 IU/dL (i.e. 57% of normal)
- A peak factor X level of 90% of normal is required in a 70 kg patient. In this situation, the appropriate dose would be:
70 kg x 90 IU/dL/{[2 IU/dL]/[IU/kg]} = 3150 IU.
The dose and frequency should be based on the individual clinical response. Patients may vary in their pharmacokinetic (e.g. half-life, in vivo recovery) and clinical responses to Coagadex. Although the dose can be estimated using the calculations above, whenever possible appropriate laboratory tests, such as serial factor X assays, should be performed to guide dose adjustments.
Control of Bleeding Episodes
Adults and adolescents aged 12 years or more for treatment of bleeding episodes: 25 IU/kg Coagadex should be injected when the first sign of bleeding occurs or just before the expected onset of menstrual bleeding. Repeat at intervals of 24 hours until the bleed stops. Judge each individual bleed on its own severity.
For secondary prophylaxis against re-bleeding or short-term prophylaxis prior to anticipated physical activity or dental appointments: 25 IU/kg Coagadex should be injected and repeated as required.
Routine prophylaxis of bleeding episodes
Due to inter-and intra-patient variability, it is recommended that trough blood levels of Factor X should be monitored at intervals, especially in the first weeks of therapy or after dosage changes. Adjust dosage regimen to clinical response and trough levels of Factor X of at least 5 IU/dL.
There are limited data on the use of Coagadex for long periods of prophylaxis in adults. There are no data available on routine prophylaxis in paediatric patients aged >12 to <18 years. 25 IU/kg twice weekly is the proposed starting dose for prophylaxis in patients >12 years of age with dose levels and dosing intervals to be adjusted as clinically indicated. Depending on individual clinical response, longer intervals, e.g. once weekly, might be adequate (see section 5.1).
Perioperative Management (Adults and adolescents aged at least 12 years of age)
Pre-surgery: calculate dose of Coagadex to raise plasma factor X levels to 70-90 IU/dL. The careful control of dose and duration of treatment is especially important in cases of major surgery.
Required dose (IU) = body weight (kg) x desired factor X rise (IU/dL) x 0.5
The desired factor X rise is the difference between the patient's plasma factor X level and the desired level, and based on the observed recovery of 2 IU/dL per IU/kg.
Example: to raise plasma factor X level from 15 IU/dL to 90 IU/dL in a 70 kg patient, the appropriate dose is:
70 x (90-15) x 0.5 = 2,625 IU.
Post-surgery: dose as necessary to maintain plasma factor X levels at a minimum of 50 IU/dL until the subject is no longer at risk of bleeding due to surgery.
It is recommended that post-infusion plasma factor X levels are measured for each patient before and after surgery, to ensure that haemostatic levels are obtained and maintained.
Elderly
No dose adjustment is necessary.
Renal impairment
No dose adjustment is necessary.
Hepatic impairment
No dose adjustment is necessary.
Paediatric population (less than 12 years of age)
For on-demand control of bleeding in children aged less than 12 years: 30 IU/kg Coagadex should be injected when the first sign of bleeding occurs. Repeat at intervals of 24 hours until the bleed stops. Judge each individual bleed on its own severity.
For secondary prophylaxis against re-bleeding or short-term prophylaxis prior to anticipated physical activity or dental appointments: 30 IU/kg Coagadex should be injected and repeated as required.
For routine prophylaxis of bleeding episodes in children aged less than 12 years: 40 IU/kg twice weekly. Due to inter-and intra-patient variability, it is recommended that trough blood levels of Factor X should be monitored at intervals, especially in the first weeks of therapy or after dosage changes. Adjust dosage regimen to clinical response and trough levels of Factor X of at least 5 IU/dL. Some patients may achieve desired FX trough levels on once weekly prophylactic therapy (see section 5.1).
For perioperative management in children aged less than 12 years: Pre-surgery: calculate dose of Coagadex to raise plasma factor X levels to 70-90 IU/dL. The careful control of dose and duration of treatment is especially important in cases of major surgery.
The expected in vivo peak increase in factor X level expressed as IU/dL (or % of normal) can be estimated using the following formulae:
Dose (IU) = body weight (kg) x desired factor X rise (IU/dL or % of normal) x 0.6
OR
Increase in factor X level (IU/dL or % of normal) = [total dose (IU)/body weight (kg)] x 1.7
Post-surgery: dose as necessary to maintain plasma factor X levels at a minimum of 50 IU/dL until the subject is no longer at risk of bleeding due to surgery.
It is recommended that post-infusion plasma factor X levels are measured for each patient before and after surgery, to ensure that haemostatic levels are obtained and maintained.
Method of administration
Intravenous use.
After reconstitution, the product should be administered by the intravenous route at a suggested rate of 10 mL/min, but no more than 20 mL/min.
For home therapy, the patient should be given appropriate training and reviewed at intervals.
For instructions on reconstitution of the medicinal product before administration, see section 6.6.
Overdose
One case of accidental overdose was reported in the clinical trials, in which a subject received approximately 80 IU/kg Coagadex to treat a bleed. No adverse events were reported relating to this overdose. There is a potential for thromboembolism with overdose.
Shelf life
Shelf life: 3 years.
After reconstitution, from a microbiological point of view, the product should be used immediately.
However, chemical and physical in-use stability has been demonstrated for 1 hour at room temperature (up to 25°C +/- 2°C).
Special precautions for storage
Do not store above 30°C.
Do not freeze.
Keep container in the outer carton in order to protect it from light.
For storage conditions after reconstitution of the medicinal product, see section 6.3.
Nature and contents of container
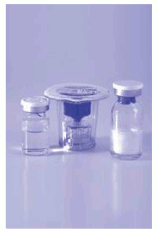
Immediate containers
Powder vial: 250 IU or 500 IU of human coagulation factor X in a type I glass vial stoppered with a halobutyl rubber stopper, oversealed with a snap-off polypropylene cap and aluminium lacquered skirt.
Solvent vial: 2.5 mL or 5 mL solution in a type I glass vial sealed with a halobutyl rubber stopper and an overseal.
Transfer Device (Mix2Vial).
Pack sizes
Coagadex 250 IU:
1 vial 250 IU human coagulation factor X powder for solution for injection
1 vial 2.5 mL water for injections
1 Transfer Device (Mix2Vial)
Coagadex 500 IU:
1 vial 500 IU human coagulation factor X powder for solution for injection
1 vial 5 mL water for injections
1 Transfer Device (Mix2Vial)
Not all pack sizes may be marketed.
Special precautions for disposal and other handling
The powder should only be reconstituted with the water for injections provided in the pack. The 250 IU and 500 IU presentations should be reconstituted using 2.5 mL and 5 mL water for injections, respectively.
Do not use the water for injections if signs of particulate matter are visible.
The vials should be brought to room temperature (not above 30°C) prior to the removal of the snap-off cap closure from the powder vial.
Step 1: Remove the cap from the powder vial and clean the top of the stopper with an alcohol swab. Repeat this step with the solvent vial. Peel back the top of the transfer device package but leave the device in the package.
Step 2: Place the blue end of the transfer device on the solvent vial and push straight down until the spike penetrates the rubber stopper and snaps into place. Remove the plastic outer packaging from the transfer device and discard it, taking care not to touch the exposed end of the device.
Step 3: Turn the solvent vial upside down with the transfer device still attached. Place the clear end of the transfer device on the powder vial and push straight down until the spike penetrates the rubber stopper and snaps into place.
Step 4: The solvent will be pulled into the powder vial by the vacuum contained within it. Gently swirl the vial to make sure the powder is thoroughly mixed. Do not shake the vial. A clear or slightly pearl-like solution should be obtained, usually in less than 1 minute (5 minutes maximum).
Step 5: Separate the empty solvent vial and blue part from the clear part by unscrewing anti-clockwise. Draw air into the syringe by pulling the plunger to the volume of water added. Connect the syringe to the clear part of the transfer device and push the air into the vial.
Step 6: Immediately invert the vial of solution, which will be drawn into the syringe. Disconnect the filled syringe from the device. Follow the normal safety practices to administer the medicine.
Note: If you have more than one vial to make up your dose, repeat steps 1 through 6 withdrawing the solution in the vial into the same syringe.
The transfer device supplied with the product is sterile and cannot be used more than once. When the reconstitution process is complete, the used transfer device should be disposed of it in the 'sharps box'.
The solution should be colourless, clear or slightly opalescent when administered. Do not use solutions that are cloudy or have deposits. Reconstituted products should be inspected visually for particulate matter and discolouration prior to administration.
Any unused product or waste material should be disposed of in accordance with local requirements.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.