ENJAYMO Solution for infusion Ref.[50928] Active ingredients: Sutimlimab
Source: European Medicines Agency (EU) Revision Year: 2023 Publisher: Sanofi B.V., Paasheuvelweg 25, 1105 BP Amsterdam, The Netherlands
5.1. Pharmacodynamic properties
Pharmacotherapeutic group: Immunosuppressants, selective immunosuppressants
ATC code: L04AA55
Mechanism of action
Sutimlimab is an IgG, subclass 4 (IgG4) monoclonal antibody (mAb) that inhibits the classical pathway (CP) and specifically binds to complement protein component 1, s subcomponent (C1s), a serine protease that cleaves C4. The activities of the lectin and alternative complement pathways are not inhibited by sutimlimab. Inhibition of the classical complement pathway at the level of C1s prevents deposition of complement opsonins on the surface of red blood cells, resulting in inhibition of haemolysis in patients with CAD, prevents generation of proinflammatory anaphylatoxins C3a and C5a and the downstream terminal complement complex C5b-9.
Clinical efficacy and safety
Greater than 90% inhibition of CP was observed after the first Enjaymo infusion and C4 levels were restored to normal levels (0.2 g/L) in CAD patients within one week following the first dose of Enjaymo.
The safety and efficacy of Enjaymo in patients with cold agglutinin disease (CAD) were assessed in a phase 3, randomized, double-blind, placebo-controlled study (CADENZA) in 42 patients (n=22 on Enjaymo and n=20 on placebo) and in a phase 3, open-label, single-arm study (CARDINAL) in 24 patients for a duration of 26 weeks. Following the completion of the six-month treatment periods (Part A), patients in both studies continued to receive Enjaymo in a long-term safety and durability of response extension phase (Part B) for an additional 12 months (CADENZA) and 24 months (CARDINAL) following last patient out from Part A. Both studies included a 9-week follow-up after the last dose of Enjaymo. Key eligibility criteria were a baseline haemoglobin (Hgb) ≤10 g/dL and active haemolysis with a bilirubin level above the normal reference range. Patients with cold agglutinin syndrome (CAS) were excluded. Patients in the CADENZA study did not have a history of transfusion within 6 months, or more than one blood transfusion in the 12 months prior to enrolment in the study while patients enrolled in the CARDINAL study had a history of at least one documented blood transfusion within 6 months prior to enrolment in the study. Patients were administered 6500 mg for 39-<75 kg or 7500 mg Enjaymo for ≥75 kg intravenously over approximately 60 minutes on Day 0, Day 7, and every 14 days thereafter. Major baseline characteristics of the study population are summarized in Table 3 below.
Table 3. Baseline characteristics of patients included in the clinical studies:
| Parameter | Statistic | CADENZA | CARDINAL | |
|---|---|---|---|---|
| Placebo N=20 | Enjaymo N=22 | Enjaymo N=24 | ||
| Age | Mean Min, Max | 68.2 51, 83 | 65.3 46, 88 | 71.3 55, 85 |
| Sex Male Female | n (%) | 4 (20.0) 16 (80.0) | 5 (22.7) 17 (77.3) | 9 (37.5) 15 (62.5) |
| Body weight | Mean, Kg Min, Max | 64.9 48, 95 | 66.8 39, 100 | 67.8 40, 112 |
| Haemoglobin | Mean, g/dL | 9.33 | 9.15 | 8.59 |
| Bilirubin (total)* | µmol/L | 35.77 (1.75 X ULN) | 41.17 (2 X ULN) | 53.26 (2.6 × ULN†) |
| History of transfusion Within last 6 months Within last 12 months | Mean number of transfusions (range) | 0 0 | 0 0.14 (0, 1) | 3.2 (1, 19) 4.8 (1, 23) |
| FACIT†-Fatigue scale | Mean | 32.99 | 31.67 | 32.5 |
* N=21 in CARDINAL; Placebo N=18 and Enjaymo N= 20 in CADENZA, for bilirubin data excluding patients with either
a positive or no available test result for Gilbert’s syndrome.
† ULN: Upper limit of normal, FACIT: Functional Assessment of Chronic Illness Therapy (FACIT-Fatigue is measured on a scale of 0 (worst fatigue) to 52 (no fatigue)
CADENZA Study
Forty-two patients were randomized to receive Enjaymo (n=22); or placebo (n=20) through Week 25. Efficacy was based on the proportion of patients who met the primary endpoint criteria: an increase from baseline in Hgb level ≥1.5 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26. A patient received a blood transfusion if they met the following haemoglobin threshold: Hgb <7 g/dL or for a Hgb <9 g/dL with symptoms. Prohibited therapies included rituximab alone or in combination with cytotoxic agents.
Efficacy was further assessed by the following two key secondary endpoints: based on the effect of Enjaymo on the mean change from baseline in Hgb and the FACIT-fatigue score to assess change in quality of life. Additional secondary endpoints were: laboratory measures of haemolysis including mean change from baseline in total bilirubin. Supportive efficacy data collected included transfusion usage after five weeks of treatment.
Efficacy results are described in Tables 4 and 5 below.
Table 4. Efficacy results in patients with CAD in the CADENZA study – Part A:
| Parameter | Statistic | Placebo N=20 | Enjaymo N=22 | Treatment effect |
|---|---|---|---|---|
| Respondera | % (95% CI) | 3 (15.0) (3.2, 37.9) | 16 (72.7) (49.8, 89.3) | |
| Odds Ratio (95% CI) | 15.94 (2.88,88.04) | |||
| p value | <0.001 | |||
| Haemoglobin | Mean change from baseline (LS† Mean), g/dL | 0.09 | 2.66 | 2.56 |
| 95% CI of LS Mean | (-0.5, 0.68) | (2.09, 3.22) | (1.75, 3.38) | |
| p value | <0.001 | |||
| Mean number of transfusions (Week 5 to Week 26) | n (SD) | 0.5 (1.1) | 0.05 (0.2) | NC |
| FACIT†-Fatigue scale | Mean | 33.66 | 43.15 | |
| Mean change from baseline (LS† Mean) | 1.91 | 10.83 | 8.93 | |
| 95% CI of LS Mean | (-1.65, 5.46) | (7.45, 14.22) | (4, 13.85) | |
| p value | <0.001 | |||
| Total bilirubin* | Mean, µmol/L | 33.95 | 12.12 | |
| Mean change from baseline | -1.83 | -22.13 | NC | |
| Number of patients normalized (%) | 4 (22.2%) | 15 (88.2) |
a A responder was defined as a patient with an increase from baseline in Hgb level ≥1.5 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26.
* N=18 for placebo and N=17 for Enjaymo, for bilirubin data excluding patients with either a positive or no available test result for Gilbert’s syndrome
† LS: Least Square, FACIT: Functional Assessment of Chronic Illness Therapy, NC= Not calculated
Mean change from baseline in haemoglobin (Hgb) is shown in the Figure 1 below.
Figure 1. CADENZA Study Part A: Plot of mean change from baseline in haemoglobin (g/dL) (+/- SE) by visit:
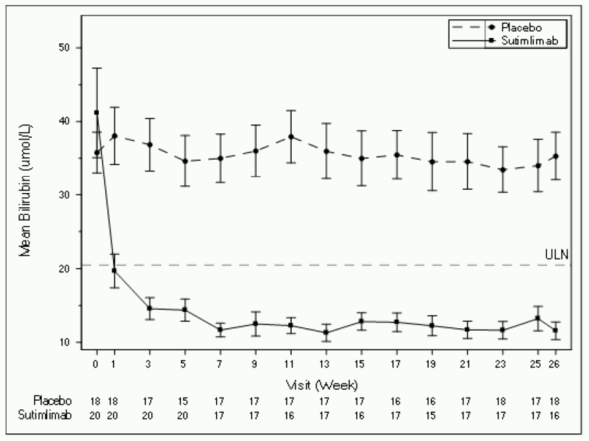
Mean bilirubin levels by visit is shown in the Figure 2 below.
Figure 2. CADENZA Study Part A: Plot of mean bilirubin (µmol/L) (+/- SE) by visit (excluding subjects with positive or unknown Gilbert’s syndrome test results):
Health-Related Quality of Life
In Part A, increases in mean FACIT-fatigue scores are presented in the Figure 3 below.
Figure 3. CADENZA Study Part A: Plot of mean change in FACIT-Fatigue score (SE) by visit – Observed – Full Analysis Set:
In Part B, mean haemoglobin levels were maintained >11 g/dL and sustained normalization of mean bilirubin levels were observed indicating a sustained decrease in haemolysis. Improvements in FACIT-Fatigue score observed in Part A were maintained.
After the last dose of Enjaymo in the study, signs and symptoms of recurrent haemolysis were observed. Mean haemoglobin, nine weeks after the last dose in Part B, decreased by 2.41 g/dL standard deviation (SD: 2.21) and mean bilirubin increased by 21.80 µmol/L (SD:18.14) from the last available values during treatment. The mean FACIT‑Fatigue score returned to near baseline levels at 31.29, with a mean SD change from baseline of -1.40 (11.48).
CARDINAL Study
Twenty-four patients were administered Enjaymo through Week 25.
Efficacy was based on the proportion of patients who met the primary endpoint criteria: an increase from baseline in Hgb level ≥2 g/dL or a Hgb level ≥12 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26. A patient received a blood transfusion if they met the following haemoglobin threshold: Hgb <7 g/dL or for a Hgb <9 g/dL with symptoms. Prohibited therapies included rituximab alone or in combination with cytotoxic agents.
Efficacy was further assessed by the following secondary endpoints: based on the effect of Enjaymo on Hgb and laboratory measures of haemolysis including mean change from baseline in total bilirubin. Change in quality of life was assessed by mean change from baseline in the FACIT-fatigue score as a secondary endpoint. Supportive efficacy data collected included transfusion usage after five weeks of treatment.
Table 5 presents efficacy results in patients with CAD in the CARDINAL study.
Table 5. Efficacy Results in Patients with CAD in the CARDINAL Study – Part A:
| Parameter | Statistic | ENJAYMO N=24 |
|---|---|---|
| Respondera | n (%) | 13 (54) |
| Haemoglobin | Mean change from baseline (LS† Mean), g/dL 95% CI of LS Mean | 2.60 (0.74, 4.46) |
| Mean number of transfusions (Week 5 to Week 26) | n | 0.9 |
| Total bilirubin* | Mean, µmol/L Mean change from baseline (LS† Mean) Number of patients normalized (%) | 15.48 (0.76 × ULN†) -38.18 13 (54.2) |
| FACIT†-Fatigue Scale | Mean Mean change from baseline (LS† Mean) 95% CI of LS Mean | 44.26 10.85 (8.0, 13.7) |
a A responder was defined as a patient with an increase from baseline in Hgb level ≥2 g/dL or a Hgb level ≥12 g/dL at the treatment assessment time point (mean value from Weeks 23, 25, and 26), no blood transfusion from Week 5 through Week 26, and no treatment for CAD beyond what was permitted per protocol from Week 5 through Week 26.
* N=21 for bilirubin data excluding patients with Gilbert’s syndrome
† LS: Least Square, ULN: Upper limit of normal, FACIT: Functional Assessment of Chronic Illness Therapy
In Part B, mean haemoglobin levels were maintained >11 g/dL and sustained normalization of mean bilirubin levels were observed indicating a sustained decrease in haemolysis.
After the last dose of Enjaymo in the study, signs and symptoms of recurrent haemolysis were observed. Mean haemoglobin, nine weeks after the last dose in Part B, decreased by 2.28 g/dL (SD: 1.80) and mean bilirubin increased by 24.27 µmol/L (SD:13.51) from the last available values during treatment. Mean FACIT-Fatigue scores returned towards baseline, with a mean SD change from baseline pre-treatment values of 1.05 (8.15).
Paediatric population
The European Medicines Agency has waived the obligation to submit the results of studies with Enjaymo in all subsets of the paediatric population in the treatment of primary Cold Agglutinin Disease (see section 4.2 for information on paediatric use).
Elderly population
Majority of the patients (43/66, 65%) included in the clinical studies with Enjaymo for CAD were 65 years of age or older. Reported clinical experience has not identified any differences in responses between those over the age of 65 and younger patients.
5.2. Pharmacokinetic properties
The pharmacokinetics (PK) of sutimlimab were characterized in 24 patients (CARDINAL) and 42 patients (CADENZA), which included 51 patients treated with 6500 mg and 15 patients with 7500 mg as per recommended posology. The total exposures at steady-state of proposed dosing regimen are presented in Table 6.
Table 6. Mean (SD) steady state exposure parameters:
| CARDINAL and CADENZA | Dose (mg) | Cmin (µg/mL)* | AUCSS (µg·h/mL)* |
|---|---|---|---|
| Mean (SD) | 6500 (n=51) 7500 (n=15) | 1397 (721) 1107 (661) | 697449 (256234) 576017 (253776) |
* Abbreviations: AUCss = area under the curve between 2 consecutive doses after steady state is achieved; Cmin = trough concentration at steady state defined as 1 hour prior to next dose administration
Steady state was achieved by week 7 after starting sutimlimab treatment, with accumulation ratio of less than 2.
Distribution
The volume of distribution at steady state in central and peripheral compartments was approximately 5.8 L in patients with CAD.
Biotransformation
Sutimlimab is a protein. It is generally recognized that antibodies are metabolized by degradation into small peptides and individual amino acids.
Elimination
The half-life of sutimlimab is dependent on the plasma concentration. The terminal elimination halflife of sutimlimab at steady-state based on the total clearance (linear and non-linear clearance) is 16 days.
Linearity/non-linearity
Following single doses, sutimlimab clearance showed a steep initial decrease at doses less than 30 mg/kg (~2 g), becoming independent of dose between 60 and 100 mg/kg of sutimlimab.
Special populations
No clinically significant differences were observed in the pharmacokinetics of sutimlimab based on sex, age, hepatic impairment, or renal impairment. Exposure levels (Cmax, Cmin and AUC) at steady state were estimated based on 6500 mg (<75 kg) and 7500 mg (>= 75 kg) given Days 0, 7 and every 14 days thereafter. The population pharmacokinetic analysis showed similar exposure parameters between sexes with 101 male and 95 female participants.
The population pharmacokinetic analysis showed similar exposure parameters with participant’s race (94 White, 10 Black, 42 Asian).
Population pharmacokinetic analysis showed that body weight and ethnicity (Japanese versus nonJapanese) influenced the pharmacokinetics of sutimlimab. Lower exposure was observed in participants with higher body weight. Based on cross-study comparison, sutimlimab AUC0-168 after 30 to 100 mg/kg was up to 38% higher in Japanese subjects than in non-Japanese participants.
Pharmacokinetic/pharmacodynamic relationship(s)
Sutimlimab concentration above 100 µg/mL resulted in maximal CP inhibition. The proposed dosing regimen resulted in adequate sutimlimab exposure at steady state to provide clinically relevant effects on Hgb, bilirubin, and total C4 levels.
5.3. Preclinical safety data
An enhanced pre- and post-natal development (ePPND) study in cynomolgus monkeys revealed no evidence of adverse developmental outcomes with intravenous administration of sutimlimab during organogenesis through delivery, at exposures approximately 2-3 times the AUC in humans at the maximum recommended dose. In repeat-dose studies with sutimlimab with exposures at up to approximately 4 times the recommended human dose, no effects on reproductive organs were observed in cynomolgus monkeys.
No animal studies have been conducted to evaluate the carcinogenic potential of sutimlimab.
Non-clinical data revealed no special hazard for humans based on nonclinical studies in cynomolgus monkeys.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.