NORVIR Film-coated tablet Ref.[107212] Active ingredients: Ritonavir
Source: European Medicines Agency (EU) Revision Year: 2023 Publisher: AbbVie Deutschland GmbH & Co. KG, Knollstrasse, 67061 Ludwigshafen, Germany
4.3. Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1.
When ritonavir is used as a pharmacokinetic enhancer of other PIs, consult the Summary of Product Characteristics of the co-administered protease inhibitor for contraindications.
Ritonavir should not be given as a pharmacokinetic enhancer or as an antiretroviral agent to patients with decompensated liver disease.
In vitro and in vivo studies have demonstrated that ritonavir is a potent inhibitor of CYP3A- and CYP2D6-mediated biotransformations. The following medicines are contraindicated when used with ritonavir and unless otherwise noted, the contraindication is based on the potential for ritonavir to inhibit metabolism of the co-administered medicinal product, resulting in increased exposure to the co-administered medicinal product and risk of clinically significant adverse effects.
The enzyme-modulating effect of ritonavir may be dose dependent. For some products, contraindications may be more relevant when ritonavir is used as an antiretroviral agent than when ritonavir is used as a pharmacokinetic enhancer (e.g. rifabutin and voriconazole):
| Medicinal Product Class | Medicinal Products within Class | Rationale |
|---|---|---|
| Concomitant medicinal product levels increased or decreased | ||
| α1-Adrenoreceptor Antagonist | Alfuzosin | Increased plasma concentrations of alfuzosin which may lead to severe hypotension (see section 4.5). |
| Analgesics | Pethidine, propoxyphene | Increased plasma concentrations of norpethidine and propoxyphene. Thereby, increasing the risk of serious respiratory depression or haematologic abnormalities, or other serious adverse effects from these agents. |
| Antianginal | Ranolazine | Increased plasma concentrations of ranolazine which may increase the potential for serious and/or life-threatening reactions (see section 4.5). |
| Anticancer | Neratinib | Increased plasma concentrations of neratinib which may increase the potential for serious and/or life-threatening reactions including hepatotoxicity (see section 4.5). |
| Venetoclax | Increased plasma concentrations of venetoclax. Increased risk of tumor lysis syndrome at the dose initiation and during the dose-titration phase (see section 4.5). | |
| Antiarrhythmics | Amiodarone, bepridil, dronedarone, encainide, flecainide, propafenone, quinidine | Increased plasma concentrations of amiodarone, bepridil, dronedarone, encainide, flecainide, propafenone, quinidine. Thereby, increasing the risk of arrhythmias or other serious adverse effects from these agents. |
| Antibiotic | Fusidic Acid | Increased plasma concentrations of fusidic acid and ritonavir. |
| Antifungal | Voriconazole | Concomitant use of ritonavir (400 mg twice daily and more) and voriconazole is contraindicated due to a reduction in voriconazole plasma concentrations and possible loss of effect (see section 4.5). |
| Antihistamines | Astemizole, terfenadine | Increased plasma concentrations of astemizole and terfenadine. Thereby, increasing the risk of serious arrhythmias from these agents. |
| Anti-gout | Colchicine | Potential for serious and/or life-threatening reactions in patients with renal and/or hepatic impairment (see sections 4.4 and 4.5). |
| Antimycobacterial | Rifabutin | Concomitant use of ritonavir (500 mg twice daily) dosed as an antiretroviral agent and rifabutin due to an increase of rifabutin serum concentrations and risk of adverse reactions including uveitis (see section 4.4). Recommendations regarding use of ritonavir dosed as a pharmacokinetic enhancer with rifabutin are noted in section 4.5. |
| Antipsychotics/ Neuroleptics | Lurasidone | Increased plasma concentrations of lurasidone which may increase the potential for serious and/or life-threatening reactions (see section 4.5). |
| Clozapine, pimozide | Increased plasma concentrations of clozapine and pimozide. Thereby, increasing the risk of serious haematologic abnormalities, or other serious adverse effects from these agents. | |
| Quetiapine | Increased plasma concentrations of quetiapine which may lead to coma. The concomitant administration with quetiapine is contraindicated (see section 4.5). | |
| Ergot Derivatives | Dihydroergotamine, ergonovine, ergotamine, methylergonovine | Increased plasma concentrations of ergot derivatives leading to acute ergot toxicity, including vasospasm and ischaemia. |
| GI motility agent | Cisapride | Increased plasma concentrations of cisapride. Thereby, increasing the risk of serious arrhythmias from this agent. |
| Lipid-modifying agents | ||
| HMG Co-A Reductase Inhibitors | Lovastatin, simvastatin | Increased plasma concentrations of lovastatin and simvastatin; thereby, increasing the risk of myopathy including rhabdomyolysis (see section 4.5). |
| Microsomal triglyceride transfer protein (MTTP) inhibitor | Lomitapide | Increased plasma concentrations of lomitapide (see section 4.5). |
| PDE5 inhibitor | Avanafil | Increased plasma concentrations of avanafil (see section 4.4. and 4.5). |
| Sildenafil | Contraindicated when used for the treatment of pulmonary arterial hypertension (PAH) only. Increased plasma concentrations of sildenafil. Thereby, increasing the potential for sildenafil- associated adverse events (which include hypotension and syncope). See section 4.4 and section 4.5 for co-administration of sildenafil in patients with erectile dysfunction. | |
| Vardenafil | Increased plasma concentrations of vardenafil (see section 4.4. and 4.5). | |
| Sedatives/hypnotics | Clorazepate, diazepam, estazolam, flurazepam, oral midazolam and triazolam | Increased plasma concentrations of clorazepate, diazepam, estazolam, flurazepam, oral midazolam and triazolam. Thereby, increasing the risk of extreme sedation and respiratory depression from these agents. (For caution on parenterally administered midazolam, see section 4.5.). |
| Ritonavir medicinal product level decreased | ||
| Herbal Preparation | St. John’s Wort | Herbal preparations containing St John’s wort (Hypericum perforatum) due to the risk of decreased plasma concentrations and reduced clinical effects of ritonavir (see section 4.5). |
4.4. Special warnings and precautions for use
Ritonavir is not a cure for HIV-1 infection or AIDS. Patients receiving Ritonavir or any other antiretroviral therapy may continue to develop opportunistic infections and other complications of HIV-1 infection.
When ritonavir is used as a pharmacokinetic enhancer with other PIs, full details on the warnings and precautions relevant to that particular PI should be considered, therefore the Summary of Product Characteristics for the particular PI must be consulted.
Ritonavir dosed as an antiretroviral agent or as a pharmacokinetic enhancer
Patients with chronic diarrhoea or malabsorption
Extra monitoring is recommended when diarrhoea occurs. The relatively high frequency of diarrhoea during treatment with ritonavir may compromise the absorption and efficacy (due to decreased compliance) of ritonavir or other concurrent medicinal products. Serious persistent vomiting and/or diarrhoea associated with ritonavir use might also compromise renal function. It is advisable to monitor renal function in patients with renal function impairment.
Haemophilia
There have been reports of increased bleeding, including spontaneous skin haematomas and haemarthroses, in haemophiliac patients type A and B treated with protease inhibitors. In some patients additional factor VIII was given. In more than a half of the reported cases, treatment with protease inhibitors was continued or reintroduced if treatment had been discontinued. A causal relationship has been evoked, although the mechanism of action has not been elucidated. Haemophiliac patients should therefore be made aware of the possibility of increased bleeding.
Weight and metabolic parameters
An increase in weight and in levels of blood lipids and glucose may occur during antiretroviral therapy. Such changes may in part be linked to disease control and life style. For lipids, there is in some cases evidence for a treatment effect, while for weight gain there is no strong evidence relating this to any particular treatment. For monitoring of blood lipids and glucose, reference is made to established HIV treatment guidelines. Lipid disorders should be managed as clinically appropriate.
Pancreatitis
Pancreatitis should be considered if clinical symptoms (nausea, vomiting, abdominal pain) or abnormalities in laboratory values (such as increased serum lipase or amylase values) suggestive of pancreatitis should occur. Patients who exhibit these signs or symptoms should be evaluated and Norvir therapy should be discontinued if a diagnosis of pancreatitis is made (see section 4.8).
Immune Reconstitution Inflammatory Syndrome
In HIV-infected patients with severe immune deficiency at the time of institution of combination antiretroviral therapy (CART), an inflammatory reaction to asymtomatic or residual opportunistic pathogens may arise and cause serious clinical conditions, or aggravation of symptoms. Typically, such reactions have been observed within the first few weeks or months of initiation of CART. Relevant examples are cytomegalovirus retinitis, generalised and/or focal mycobacterial infections, and Pneumocystis jiroveci pneumonia. Any inflammatory symptoms should be evaluated and treatment instituted when necessary.
Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported to occur in the setting of immune reconstitution; however, the reported time to onset is more variable and can occur many months after initiation of treatment.
Liver disease
Ritonavir should not be given to patients with decompensated liver disease (see section 4.2). Patients with chronic hepatitis B or C and treated with combination antiretroviral therapy are at an increased risk for severe and potentially fatal hepatic adverse reactions. In case of concomitant antiviral therapy for hepatitis B or C, please refer to the relevant product information for these medicinal products.
Patients with pre-existing liver dysfunction including chronic active hepatitis have an increased frequency of liver function abnormalities during combination antiretroviral therapy and should be monitored according to standard practice. If there is evidence of worsening liver disease in such patients, interruption or discontinuation of treatment must be considered.
Renal disease
Since the renal clearance of ritonavir is negligible, the decrease in the total body clearance is not expected in patients with renal impairment (see also section 4.2).
Renal failure, renal impairment, elevated creatinine, hypophosphataemia and proximal tubulopathy (including Fanconi syndrome) have been reported with the use of tenofovir disoproxil fumarate (DF) in clinical practice (see section 4.8).
Osteonecrosis
Although the aetiology is considered to be multifactorial (including corticosteroid use, alcohol consumption, severe immunosuppression, higher body mass index), cases of osteonecrosis have been reported in patients with advanced HIV-disease and/or long-term exposure to combination antiretroviral therapy (CART). Patients should be advised to seek medical advice if they experience joint aches and pain, joint stiffness or difficulty in movement.
PR interval prolongation
Ritonavir has been shown to cause modest asymptomatic prolongation of the PR interval in some healthy adult subjects. Rare reports of 2nd or 3rd degree atrioventricular block in patients with underlying structural heart disease and pre-existing conduction system abnormalities or in patients receiving medicinal products known to prolong the PR interval (such as verapamil or atazanavir) have been reported in patients receiving ritonavir. Norvir should be used with caution in such patients (see section 5.1).
Interactions with other medicinal products
Ritonavir dosed as an antiretroviral agent
The following warnings and precautions should be considered when ritonavir is used as an antiretroviral agent. When ritonavir is used as a pharmacokinetic enhancer at the 100 mg and 200 mg level it cannot be assumed that the following warnings and precautions will also apply. When ritonavir is used as a pharmacokinetic enhancer, full details on the warnings and precautions relevant to that particular PI must be considered, therefore the Summary of Product Characteristics, section 4.4, for the particular PI must be consulted to determine if the information below is applicable.
PDE5 inhibitors
Particular caution should be used when prescribing sildenafil or tadalafil for the treatment of erectile dysfunction in patients receiving ritonavir. Co-administration of ritonavir with these medicinal products is expected to substantially increase their concentrations and may result in associated adverse reactions such as hypotension and prolonged erection (see section 4.5). Concomitant use of avanafil or vardenafil with ritonavir is contraindicated (see section 4.3). Concomitant use of sildenafil with ritonavir is contraindicated in pulmonary arterial hypertension patients (see section 4.3).
HMG-CoA reductase inhibitors
The HMG-CoA reductase inhibitors simvastatin and lovastatin are highly dependent on CYP3A for metabolism, thus concomitant use of ritonavir with simvastatin or lovastatin is not recommended due to an increased risk of myopathy including rhabdomyolysis. Caution must also be exercised and reduced doses should be considered if ritonavir is used concurrently with atorvastatin, which is metabolised to a lesser extent by CYP3A. While rosuvastatin elimination is not dependent on CYP3A, an elevation of rosuvastatin exposure has been reported with ritonavir co-administration. The mechanism of this interaction is not clear, but may be the result of transporter inhibition. When used with ritonavir dosed as a pharmacokinetic enhancer or as an antiretroviral agent, the lowest doses of atorvastatin or rosuvastatin should be administered. The metabolism of pravastatin and fluvastatin is not dependent of CYP3A, and interactions are not expected with ritonavir. If treatment with an HMGCoA reductase inhibitor is indicated, pravastatin or fluvastatin is recommended (see section 4.5).
Colchicine
Life-threatening and fatal drug interactions have been reported in patients treated with colchicine and strong inhibitors of CYP3A like ritonavir (see sections 4.3 and 4.5).
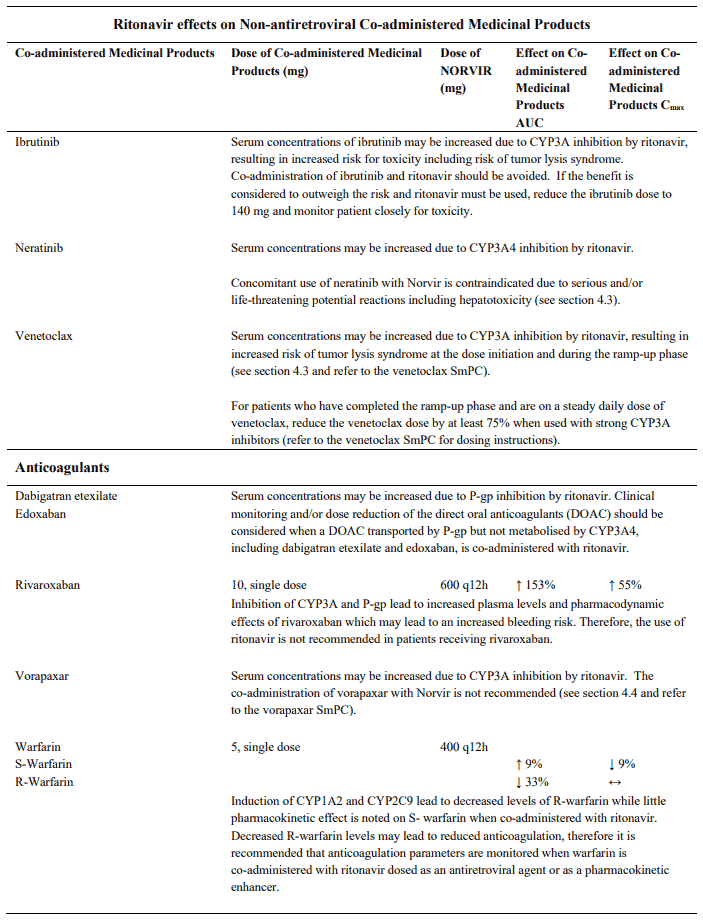
Digoxin
Particular caution should be used when prescribing ritonavir in patients taking digoxin since co-administration of ritonavir with digoxin is expected to increase digoxin levels. The increased digoxin levels may lessen over time (see section 4.5).
In patients who are already taking digoxin when ritonavir is introduced, the digoxin dose should be reduced to one-half of the patients' normal dose and patients need to be followed more closely than usual for several weeks after initiating co-administration of ritonavir and digoxin.
In patients who are already taking ritonavir when digoxin is introduced, digoxin should be introduced more gradually than usual. Digoxin levels should be monitored more intensively than usual during this period, with dose adjustments made, as necessary, based on clinical, electrocardiographic and digoxin level findings.
Ethinyl estradiol
Barrier or other non-hormonal methods of contraception should be considered when administering ritonavir at therapeutic or low doses as ritonavir is likely to reduce the effect and change the uterine bleeding profile when co-administered with estradiol-containing contraceptives.
Glucocorticoids
Concomitant use of ritonavir and fluticasone or other glucocorticoids that are metabolised by CYP3A4 is not recommended unless the potential benefit of treatment outweighs the risk of systemic corticosteroid effects, including Cushing’s syndrome and adrenal suppression (see section 4.5).
Trazodone
Particular caution should be used when prescribing ritonavir in patients using trazodone. Trazodone is a CYP3A4 substrate and co-administration of ritonavir is expected to increase trazodone levels. Adverse reactions of nausea, dizziness, hypotension and syncope have been observed in single dose interaction studies in healthy volunteers (see section 4.5).
Rivaroxaban
It is not recommended to use ritonavir in patients receiving rivaroxaban, due to the risk of increased bleeding (see section 4.5).
Riociguat
The concomitant use of ritonavir is not recommended due to potential increase in riociguat exposure (see section 4.5).
Vorapaxar
The concomitant use of ritonavir is not recommended due to potential increase in vorapaxar exposure (see section 4.5).
Bedaquiline
Strong CYP3A4 inhibitors such as protease inhibitors may increase bedaquiline exposure which could potentially increase the risk of bedaquiline-related adverse reactions. Therefore, combination of bedaquiline with ritonavir should be avoided. However, if the benefit outweighs the risk, coadministration of bedaquiline with ritonavir must be done with caution. More frequent electrocardiogram monitoring and monitoring of transaminases is recommended (see section 4.5 and refer to the bedaquiline Summary of Product Characteristics).
Delamanid
Co-administration of delamanid with a strong inhibitor of CYP3A (ritonavir) may increase exposure to delamanid metabolite, which has been associated with QTc prolongation. Therefore, if co-administration of delamanid with ritonavir is considered necessary, very frequent ECG monitoring throughout the full delamanid treatment period is recommended (see section 4.5 and refer to the delamanid Summary of Product Characteristics).
Ritonavir dosed as a pharmacokinetic enhancer
The interaction profiles of HIV-protease inhibitors, co-administered with low dose ritonavir, are dependant on the specific co-administered protease inhibitor.
For a description of the mechanisms and potential mechanisms contributing to the interaction profile of the PIs, see section 4.5. Please also review the Summary of Product Characteristics for the particular boosted PI.
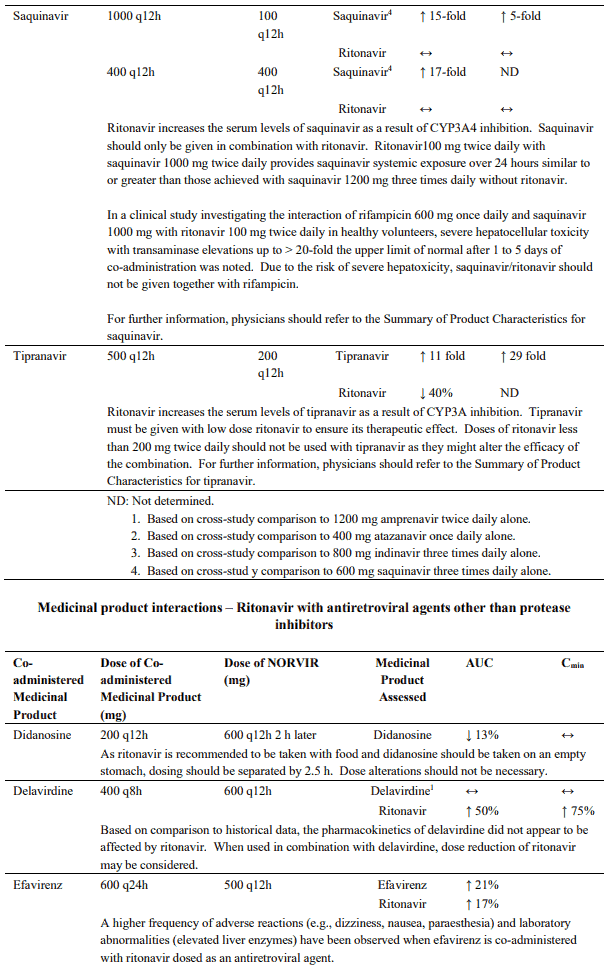
Saquinavir
Doses of ritonavir higher than 100 mg twice daily should not be used. Higher doses of ritonavir have been shown to be associated with an increased incidence of adverse reactions. Co-administration of saquinavir and ritonavir has led to severe adverse reactions, mainly diabetic ketoacidosis and liver disorders, especially in patients with pre-existing liver disease.
Saquinavir/ritonavir should not be given together with rifampicin, due to the risk of severe hepatotoxicity (presenting as increased hepatic transaminases) if the three medicines are given together (see section 4.5).
Tipranavir
Co-administration of tipranavir with 200 mg of ritonavir has been associated with reports of clinical hepatitis and hepatic decompensation including some fatalities. Extra vigilance is warranted in patients with chronic hepatitis B or hepatitis C co-infection, as these patients have an increased risk of hepatotoxicity.
Doses of ritonavir lower than 200 mg twice daily should not be used as they might alter the efficacy profile of the combination.
Fosamprenavir
Co-administration of fosamprenavir with ritonavir in doses greater than 100 mg twice daily has not been clinically evaluated. The use of higher ritonavir doses might alter the safety profile of the combination and therefore is not recommended.
Atazanavir
Co-administration of atazanavir with ritonavir at doses greater than 100 mg once daily has not been clinically evaluated. The use of higher ritonavir doses may alter the safety profile of atazanavir (cardiac effects, hyperbilirubinemia) and therefore is not recommended. Only when atazanavir with ritonavir is co-administered with efavirenz, a dose increase of ritonavir to 200mg once daily could be considered. In this instance, close clinical monitoring is warranted. Refer to the Summary of Product Characteristics for atazanavir for further details.
Sodium
This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodiumfree’.
4.5. Interaction with other medicinal products and other forms of interaction
Ritonavir dosed as a pharmacokinetic enhancer or as an antiretroviral agent
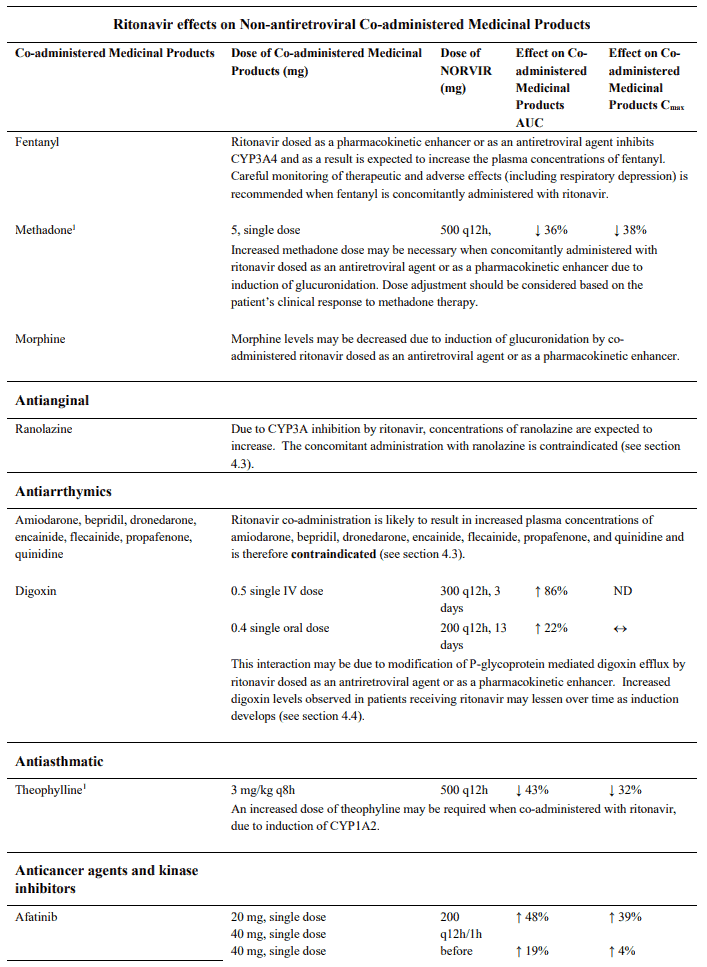
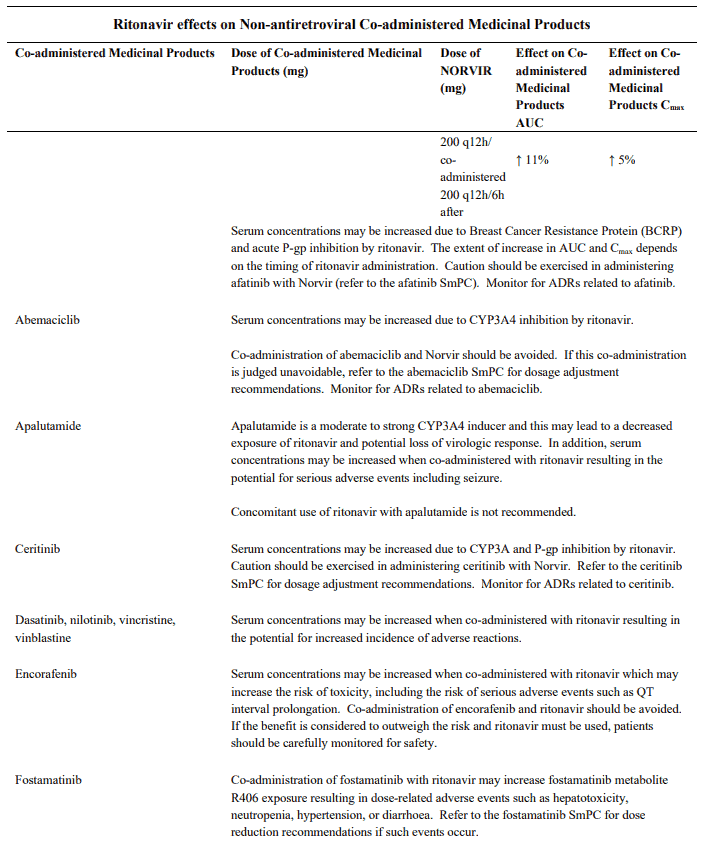
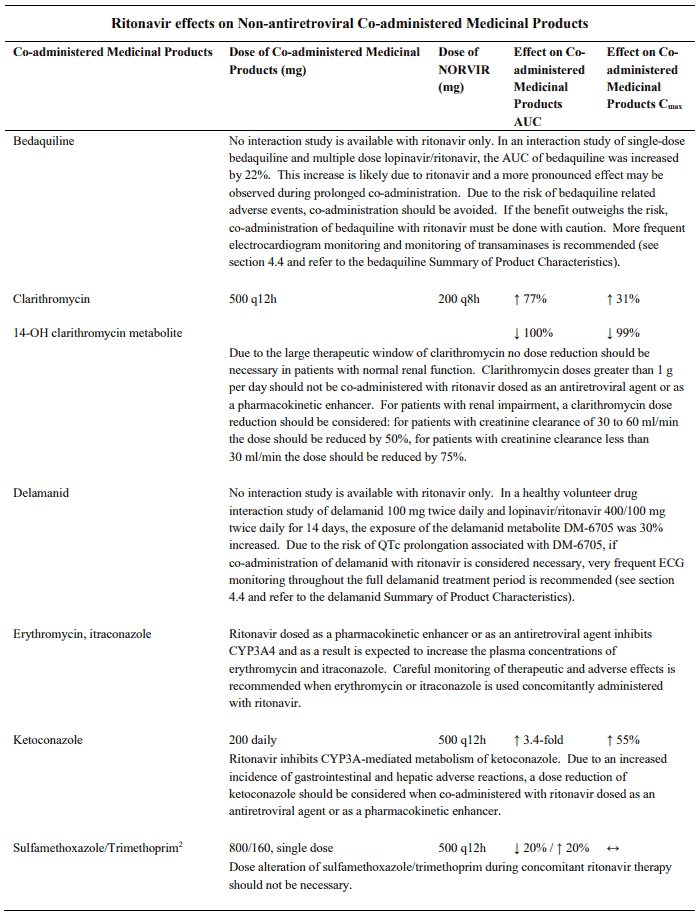
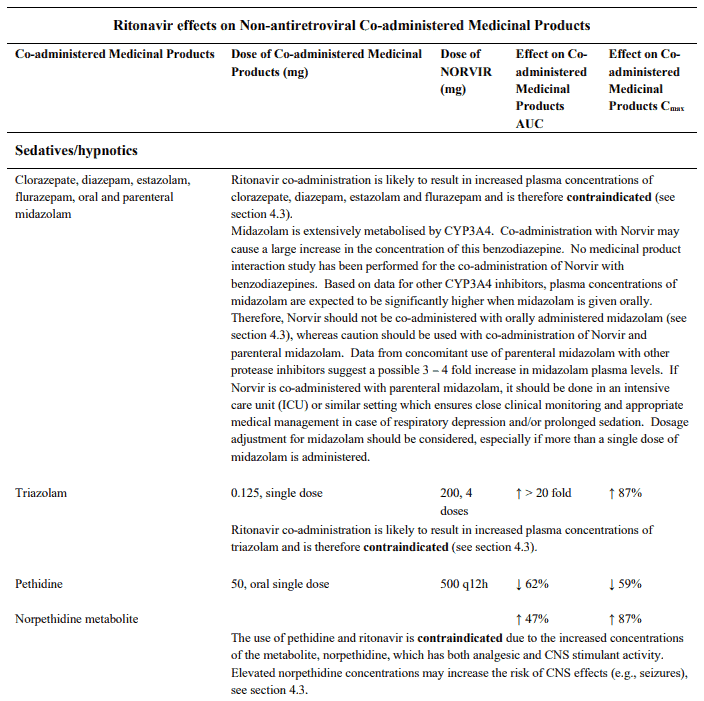
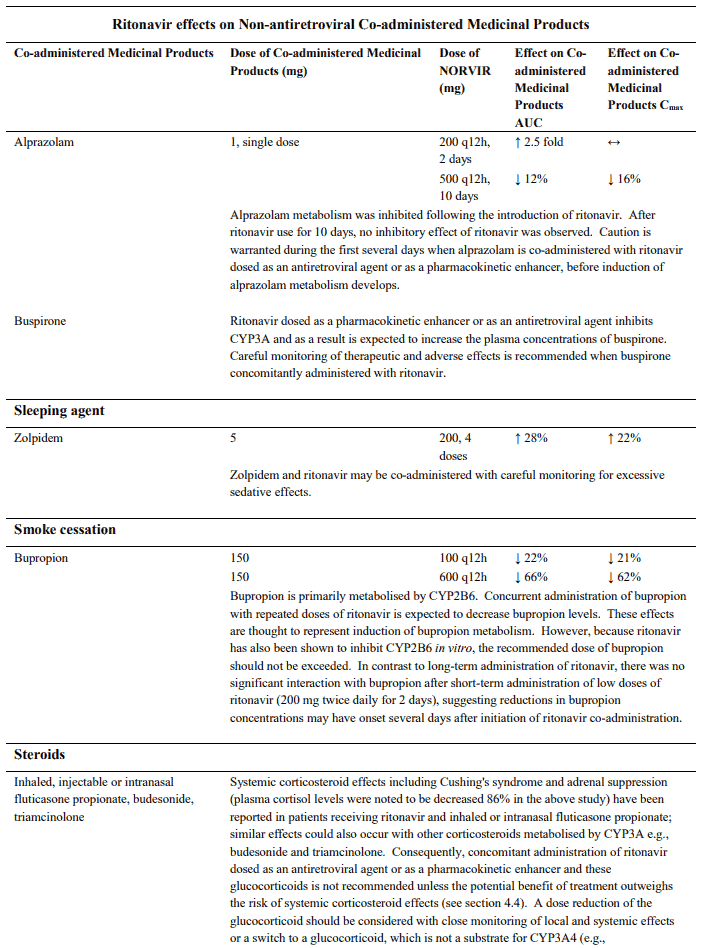
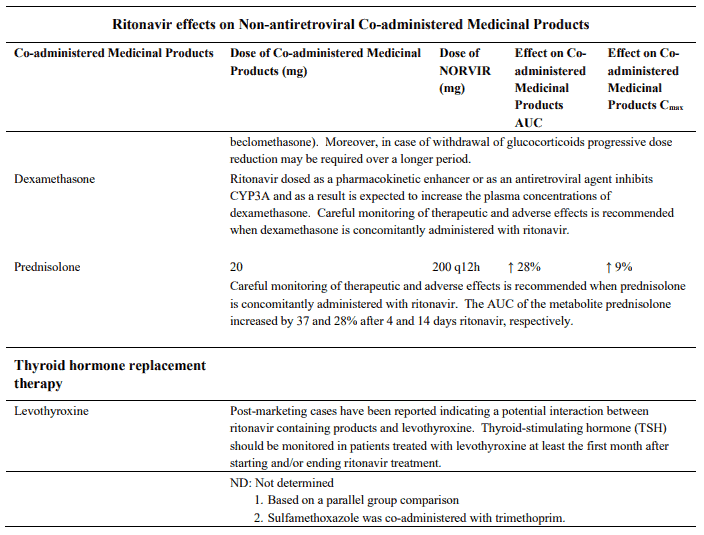
Ritonavir has a high affinity for several cytochrome P450 (CYP) isoforms and may inhibit oxidation with the following ranked order: CYP3A4 > CYP2D6. Co-administration of ritonavir and medicinal products primarily metabolised by CYP3A may result in increased plasma concentrations of the other medicinal product, which could increase or prolong its therapeutic and adverse effects. For selected medicinal products (e.g. alprazolam) the inhibitory effects of ritonavir on CYP3A4 may decrease over time. Ritonavir also has a high affinity for P-glycoprotein and may inhibit this transporter. The inhibitory effect of ritonavir (with or without other protease inhibitors) on P-gp activity may decrease over time (e.g. digoxin and fexofenadine-see table “Ritonavir effects on non-antiretroviral medicinal products” below). Ritonavir may induce glucuronidation and oxidation by CYP1A2, CYP2C8, CYP2C9 and CYP2C19 thereby increasing the biotransformation of some medicinal products metabolised by these pathways, and may result in decreased systemic exposure to such medicinal products, which could decease or shorten their therapeutic effect.
Important information regarding medicinal product interactions when ritonavir is used as a pharmacokinetic enhancer is also contained in the Summary of Product Characteristics of the co-administered protease inhibitor.
Medicinal products that affect ritonavir levels
Serum levels of ritonavir can be reduced by concomitant use of herbal preparations containing St John’s wort (Hypericum perforatum). This is due to the induction of medicinal product metabolising enzymes by St John’s wort. Herbal preparations containing St John’s wort must not be used in combination with ritonavir. If a patient is already taking St John’s wort, St John’s wort should be stopped and if possible check viral levels. Ritonavir levels may increase on stopping St John’s wort. The dose of ritonavir may need adjusting. The inducing effect may persist for at least 2 weeks after cessation of treatment with St John’s wort (see section 4.3).
Serum levels of ritonavir may be affected by select co-administered medicinal products (e.g. delavirdine, efavirenz, phenytoin and rifampicin). These interactions are noted in the medicinal product interaction tables below.
Medicinal products that are affected by the use of ritonavir
Interactions between ritonavir and protease inhibitors, antiretroviral agents other than protease inhibitors and other non-antiretroviral medicinal products are listed in the tables below. This list is not intended to be inclusive or comprehensive. Individual SmPCs should be consulted.
Cardiac and neurologic events have been reported when ritonavir has been co-administered with disopyramide, mexiletine or nefazodone. The possibility of medicinal product interaction cannot be excluded.
In addition to the interactions listed above, as ritonavir is highly protein bound, the possibility of increased therapeutic and toxic effects due to protein binding displacement of concomitant medicinal products should be considered.
Ritonavir dosed as a pharmacokinetic enhancer
Important information regarding medicinal product interactions when ritonavir is used a pharmacokinetic enhancer is also contained in the Summary of Product Characteristics of the coadministered protease inhibitor.
Proton pump inhibitors and H2-receptor antagonists
Proton pump inhibitors and H2-receptor antagonists (e.g. omeprazole or ranitidine) may reduce concentrations for co-administered protease inhibitors. For specific information regarding the impact of co-administration of acid reducing agents, refer to the Summary of Product Characteristics of the co-administered protease inhibitor. Based on interaction studies with the ritonavir boosted protease inhibitors (lopinavir/ritonavir, atazanavir), concurrent administration of omeprazole or ranitidine does not significantly modify ritonavir efficacy as a pharmacokinetic enhancer despite a slight change of exposure (about 6-18%).
4.6. Fertility, pregnancy and lactation
Pregnancy
A large amount (6100 live births) of pregnant women were exposed to ritonavir during pregnancy; of these, 2800 live births were exposed during the first trimester. These data largely refer to exposures where ritonavir was used in combination therapy and not at therapeutic ritonavir doses but at lower doses as a pharmacokinetic enhancer for other PIs. These data indicate no increase in the rate of birth defects compared to rates observed in population-based birth defect surveillance systems. Animal data have shown reproductive toxicity (see section 5.3). Norvir can be used during pregnancy if clinically needed.
Ritonavir adversely interacts with oral contraceptives (OCs). Therefore, an alternative, effective and safe method of contraception should be used during treatment.
Breast-feeding
Limited published data reports that ritonavir is present in human milk. There is no information on the effects of ritonavir on the breastfed infant or the effects of the drug on milk production. Because of the potential for (1) HIV transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants) and (3) serious adverse reactions in a breastfed infant, women living with HIV should not breast-feed their infants if they are receiving Norvir.
Fertility
No human data on the effect of ritonavir on fertility are available. Animal studies do not indicate harmful effects of ritonavir on fertility (see section 5.3).
4.7. Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. Dizziness is a known undesirable effect that should be taken into account when driving or using machinery.
4.8. Undesirable effects
Summary of the safety profile
Ritonavir dosed as a pharmacokinetic enhancer
Adverse reactions associated with the use of ritonavir as a pharmacokinetic enhancer are dependent on the specific co-administered PI. For information on adverse reactions refer to the SPC of the specific co-administered PI.
Ritonavir dosed as an antiretroviral agent
Adverse reactions from clinical trials and post-marketing experience in adult patients
The most frequently reported adverse drug reactions among patients receiving ritonavir alone or in combination with other antiretroviral drugs were gastrointestinal (including diarrhea, nausea, vomiting, abdominal pain (upper and lower)), neurological disturbances (including paresthesia and oral paresthesia) and fatigue/asthenia.
Tabulated list of adverse reactions
The following adverse reactions of moderate to severe intensity with possible or probable relationship to ritonavir have been reported. Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1000 to <1/100); rare (≥1/10,000 to <1/1,000); not known (cannot be estimated from the available data).
Events noted as having frequency not known were identified via post-marketing surveillance.
Adverse reactions in clinical studies and post-marketing in adult patients:
| System Order Class | Frequency | Adverse reaction |
|---|---|---|
| Blood and lymphatic system disorders | Common | Decreased white blood cells, decreased haemoglobin, decreased neutrophils, increased eosinophils, thrombocytopenia |
| Uncommon | Increased neutrophils | |
| Immune system disorders | Common | Hypersensitivity including urticaria, and face oedema |
| Rare | Anaphylaxis | |
| Metabolism and nutrition disorders | Common | Hypercholesterolaemia, hypertriglyceridaemia, gout, oedema and peripheral oedema, dehydration (usually associated with gastrointestinal symptoms) |
| Uncommon | Diabetes mellitus | |
| Rare | Hyperglycaemia | |
| Nervous system disorders | Very common | Dysgeusia, oral and peripheral paraesthesia, headache, dizziness, peripheral neuropathy |
| Common | Insomnia, anxiety, confusion, disturbance in attention, syncope, seizure | |
| Eye disorders | Common | Blurred vision |
| Cardiac disorders | Uncommon | Myocardial infarction |
| Vascular disorders | Common | Hypertension, hypotension including orthostatic hypotension, peripheral coldness |
| Respiratory, thoracic and mediastinal disorders | Very common | Pharyngitis, oropharyngeal pain, cough |
| Gastrointestinal disorders | Very common | Abdominal pain (upper and lower), nausea, diarrhoea (including severe with electrolyte imbalance), vomiting, dyspepsia |
| Common | Anorexia, flatulence, mouth ulcer, gastrointestinal haemorrhage, gastroesophageal reflux disease, pancreatitis | |
| Hepatobiliary disorders | Common | Hepatitis (including increased AST, ALT, GGT), blood bilirubin increased (including jaundice) |
| Skin and subcutaneous tissue disorders | Very common | Pruritus, rash (including erythematous and maculopapular) |
| Common | Acne | |
| Rare | Stevens Johnson syndrome, toxic epidermal necrolysis (TEN) | |
| Musculosketal and connective tissue disorders | Very common | Arthralgia and back pain |
| Common | Myositis, rhabdomyolysis, myalgia, myopathy/CPK increased | |
| Renal and urinary disorders | Common | Increased urination, renal impairment (e.g. oliguria, elevated creatinine) |
| Uncommon | Acute renal failure | |
| Not known | Nephrolithiasis | |
| Reproductive system and breast disorders | Common | Menorrhagia |
| General disorders and administration site conditions | Very common | Fatigue including asthenia, flushing, feeling hot |
| Common | Fever, weight loss | |
| Investigations | Common | Increased amylase, decreased free and total thyroxin |
| Uncommon | Increased glucose, increased magnesium, increased alkaline phosphatase |
Description of selected adverse reactions
Hepatic transaminase elevations exceeding five times the upper limit or normal, clinical hepatitis, and jaundice have occurred in patients receiving ritonavir alone or in combination with other antiretrovirals.
Metabolic parameters
Weight and levels of blood lipids and glucose may increase during antiretroviral therapy (see section 4.4).
In HIV-infected patients with severe immune deficiency at the time of initiation of combination antiretroviral therapy (CART), an inflammatory reaction to asymptomatic or residual opportunistic infections may arise. Autoimmune disorders (such as Graves' disease and autoimmune hepatitis) have also been reported; however, the reported time to onset is more variable and can occur many months after initiation of treatment (see section 4.4).
Pancreatitis has been observed in patients receiving ritonavir therapy, including those who developed hypertriglyceridemia. In some cases fatalities have been observed. Patients with advanced HIV disease may be at risk of elevated triglycerides and pancreatitis (see section 4.4).
Cases of osteonecrosis have been reported, particularly in patients with generally acknowledged risk factors, advanced HIV disease or long-term exposure to combination antiretroviral therapy (CART). The frequency of this is unknown (see section 4.4).
Paediatric populations
The safety profile of Norvir in children 2 years of age and older is similar to that seen in adults.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V.
6.2. Incompatibilities
Not applicable.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.