VENCLEXTA Film coated tablet Ref.[11111] Active ingredients: Venetoclax
Source: FDA, National Drug Code (US) Revision Year: 2020
12.1. Mechanism of Action
Venetoclax is a selective and orally bioavailable small-molecule inhibitor of BCL-2, an anti-apoptotic protein. Overexpression of BCL-2 has been demonstrated in CLL and AML cells where it mediates tumor cell survival and has been associated with resistance to chemotherapeutics. Venetoclax helps restore the process of apoptosis by binding directly to the BCL-2 protein, displacing pro-apoptotic proteins like BIM, triggering mitochondrial outer membrane permeabilization and the activation of caspases. In nonclinical studies, venetoclax has demonstrated cytotoxic activity in tumor cells that overexpress BCL-2.
12.2. Pharmacodynamics
Based on the exposure response analyses for efficacy, a relationship between drug exposure and a greater likelihood of response was observed in clinical studies in patients with CLL/SLL, and in patients with AML. Based on the exposure response analyses for safety, a relationship between drug exposure and a greater likelihood of some safety events was observed in clinical studies in patients with AML. No exposure-safety relationship was observed in patients with CLL/SLL at doses up to 1200 mg given as monotherapy and up to 600 mg given in combination with rituximab.
Cardiac Electrophysiology
The effect of multiple doses of VENCLEXTA up to 1200 mg once daily (2 times the maximum approved recommended dosage) on the QTc interval was evaluated in an open-label, single-arm trial in 176 patients with previously treated hematologic malignancies. VENCLEXTA had no large effect on QTc interval (i.e., >20 ms) and there was no relationship between venetoclax exposure and change in QTc interval.
12.3. Pharmacokinetics
Venetoclax mean (± standard deviation) steady state Cmax was 2.1 ± 1.1 mcg/mL and AUC0-24h was 32.8 ± 16.9 mcg•h/mL following administration of 400 mg once daily with a low-fat meal. Venetoclax steady state AUC increased proportionally over the dose range of 150 to 800 mg (0.25 to 1.33 times the maximum approved recommended dosage). The pharmacokinetics of venetoclax does not change over time.
Absorption
Maximum plasma concentration of venetoclax was reached 5 to 8 hours following multiple oral administration under fed conditions.
Effect of Food
Administration with a low-fat meal (approximately 512 kilocalories, 25% fat calories, 60% carbohydrate calories, and 15% protein calories) increased venetoclax exposure by approximately 3.4-fold and administration with a high-fat meal (approximately 753 kilocalories, 55% fat calories, 28% carbohydrate calories, and 17% protein calories) increased venetoclax exposure by 5.1- to 5.3-fold compared with fasting conditions.
Distribution
Venetoclax is highly bound to human plasma protein with unbound fraction in plasma <0.01 across a concentration range of 1-30 micromolar (0.87-26 mcg/mL). The mean blood-to-plasma ratio was 0.57. The apparent volume of distribution (Vdss/F) of venetoclax ranged from 256-321 L in patients.
Elimination
The terminal elimination half-life of venetoclax was approximately 26 hours.
Metabolism
Venetoclax is predominantly metabolized by CYP3A in vitro. The major metabolite identified in plasma, M27, has an inhibitory activity against BCL-2 that is at least 58-fold lower than venetoclax in vitro and its AUC represented 80% of the parent AUC.
Excretion
After single oral dose of radiolabeled [14C]-venetoclax 200 mg to healthy subjects, >99.9% of the dose was recovered in feces (21% as unchanged) and <0.1% in urine within 9 days.
Specific Populations
No clinically significant differences in the pharmacokinetics of venetoclax were observed based on age (19 to 93 years), sex, weight, mild to severe renal impairment (CLcr 15 to 89 mL/min, calculated by Cockcroft-Gault), or mild to moderate hepatic impairment (normal total bilirubin and aspartate transaminase (AST) > upper limit of normal (ULN) or total bilirubin 1 to 3 times ULN). The effect of end-stage renal disease (CLcr <15 mL/min) or dialysis on venetoclax pharmacokinetics is unknown.
Racial or Ethnic Groups
No clinically significant differences in the pharmacokinetics of venetoclax were observed in White, Black, and Asian patients enrolled in the United States. Of 771 patients with AML, Asian patients from Asian countries [China (5.6%), Japan (5.5%), South Korea (2.1%), and Taiwan (0.9%)] had 63% higher venetoclax exposure than non-Asian populations.
Patients with Hepatic Impairment
Following a single dose of VENCLEXTA 50 mg, venetoclax systemic exposure (AUC0-INF) was 2.7-fold higher in subjects with severe hepatic impairment (Child-Pugh C) compared to subjects with normal hepatic function [see Dosage and Administration (2.7) and Use in Specific Populations (8.7)]. No clinically relevant differences in venetoclax systemic exposure were observed between subjects with mild or moderate hepatic impairment and subjects with normal hepatic function.
Drug Interactions Studies
Clinical Studies
No clinically significant differences in venetoclax pharmacokinetics were observed when coadministered with azacitidine, azithromycin, cytarabine, decitabine, gastric acid reducing agents, obinutuzumab, or rituximab.
Ketoconazole:
Concomitant use of ketoconazole (a strong CYP3A, P-gp, and BCRP inhibitor) 400 mg once daily for 7 days increased venetoclax Cmax by 130% and AUC0-INF by 540% [see Drug Interactions (7.1)].
Ritonavir:
Concomitant use of ritonavir (a strong CYP3A, P-gp, and OATP1B1/B3 inhibitor) 50 mg once daily for 14 days increased venetoclax Cmax by 140% and AUC by 690% [see Drug Interactions (7.1)].
Posaconazole:
Concomitant use of posaconazole (a strong CYP3A and P-gp inhibitor) 300 mg with VENCLEXTA 50 mg and 100 mg for 7 days resulted in 61% and 86% higher venetoclax Cmax, respectively, compared with VENCLEXTA 400 mg administered alone. The venetoclax AUC0-24h was 90% and 144% higher, respectively [see Drug Interactions (7.1)].
Rifampin:
Concomitant use of a single dose of rifampin (an OATP1B1/1B3 and P-gp inhibitor) 600 mg increased venetoclax Cmax by 106% and AUC0-INF by 78%. Concomitant use of multiple doses of rifampin (as a strong CYP3A inducer) 600 mg once daily for 13 days decreased venetoclax Cmax by 42% and AUC0-INF by 71% [see Drug Interactions (7.1)].
Warfarin:
Concomitant use of a single 400 mg dose of VENCLEXTA with 5 mg of warfarin resulted in 18% to 28% increase in Cmax and AUC0-INF of R-warfarin and S-warfarin [see Drug Interactions (7.2)].
Digoxin:
Concomitant use of a single dose of VENCLEXTA 100 mg with digoxin (a P-gp substrate) 0.5 mg increased digoxin Cmax by 35% and AUC0-INF by 9% [see Drug Interactions (7.2)].
In Vitro Studies
Venetoclax is not an inhibitor or inducer of CYP1A2, CYP2B6, CYP2C19, CYP2D6, or CYP3A4. Venetoclax is a weak inhibitor of CYP2C8, CYP2C9, and UGT1A1.
Venetoclax is not an inhibitor of UGT1A4, UGT1A6, UGT1A9, or UGT2B7.
Venetoclax is an inhibitor and substrate of P-gp and BCRP and weak inhibitor of OATP1B1.
Venetoclax is not an inhibitor of OATP1B3, OCT1, OCT2, OAT1, OAT3, MATE1, or MATE2K.
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Neither venetoclax nor M27, a major human metabolite, were carcinogenic in a 6-month transgenic (Tg.rasH2) mouse study at oral doses up to 400 mg/kg/day of venetoclax, and at a single oral dose level of 250 mg/kg/day of M27.
Venetoclax was not mutagenic in an in vitro bacterial mutagenicity (Ames) assay, did not induce numerical or structural aberrations in an in vitro chromosome aberration assay using human peripheral blood lymphocytes, and was not clastogenic in an in vivo mouse bone marrow micronucleus assay at doses up to 835 mg/kg. The M27 metabolite was negative for genotoxic activity in in vitro Ames and chromosome aberration assays.
Fertility and early embryonic development studies were conducted in male and female mice. These studies evaluate mating, fertilization, and embryonic development through implantation. There were no effects of venetoclax on estrous cycles, mating, fertility, corpora lutea, uterine implants or live embryos per litter at dosages up to 600 mg/kg/day. However, a risk to human male fertility exists based on testicular toxicity (germ cell loss) observed in dogs at exposures as low as 0.5 times the human AUC exposure at a dose of 400 mg.
13.2. Animal Toxicology and/or Pharmacology
In dogs, venetoclax caused single-cell necrosis in various tissues, including the gallbladder, exocrine pancreas, and stomach with no evidence of disruption of tissue integrity or organ dysfunction; these findings were minimal to mild in magnitude. Following a 4-week dosing period and subsequent 4-week recovery period, minimal single-cell necrosis was still present in some tissues and reversibility has not been assessed following longer periods of dosing or recovery.
In addition, after approximately 3 months of daily dosing in dogs, venetoclax caused progressive white discoloration of the hair coat due to loss of melanin pigment.
14. Clinical Studies
14.1 Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
In Combination with Obinutuzumab
CLL14 (BO25323) was a randomized (1:1), multicenter, open-label, actively controlled trial (NCT02242942) that evaluated the efficacy and safety of VENCLEXTA in combination with obinutuzumab (VEN+G) versus obinutuzumab in combination with chlorambucil (GClb) for patients with previously untreated CLL with coexisting medical conditions (total Cumulative Illness Rating Scale [CIRS] score >6 or CLcr <70 mL/min). The trial required hepatic transaminases and total bilirubin ≤2 times upper limit of normal and excluded patients with Richter's transformation or any individual organ/system impairment score of 4 by CIRS except eye, ear, nose, and throat organ system.
All patients received obinutuzumab at 1000 mg on Days 1 (the first dose could be split as 100 mg and 900 mg on Days 1 and 2), 8 and 15 of Cycle 1, and on Day 1 of each subsequent cycle for a total of 6 cycles. Patients in the VEN+G arm began the VENCLEXTA 5-week ramp-up dosing schedule [see Dosage and Administration (2.2, 2.4)] on Day 22 of Cycle 1 and received VENCLEXTA 400 mg orally once daily from Cycle 3 Day 1 until the last day of Cycle 12. Patients randomized to the GClb arm received chlorambucil 0.5 mg/kg orally on Day 1 and Day 15 of Cycles 1 to 12. Each cycle was 28 days.
A total of 432 patients were randomized, 216 to each arm. Baseline demographic and disease characteristics were similar between the arms. The median age was 72 years (range: 41 to 89 years), 89% were White, 67% were male; 36% and 43% were Binet stage B and C, respectively, and 88% had Eastern Cooperative Oncology Group (ECOG) performance status <2. The median CIRS score was 8.0 (range: 0 to 28) and 58% of patients had CLcr <70 mL/min. A 17p deletion was detected in 8% of patients, TP53 mutations in 10%, 11q deletion in 19%, and unmutated IgVH in 57%.
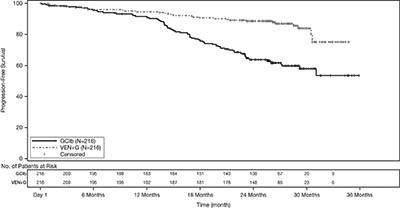
Efficacy was based on progression-free survival (PFS) as assessed by an Independent Review Committee (IRC). The median duration of follow-up for PFS was 28 months (range: 0 to 36 months). Efficacy results for CLL14 are shown in Table 19. The Kaplan-Meier curve for PFS is shown in Figure 1.
Table 19. Efficacy Results in CLL14:
| Endpoint | VENCLEXTA + Obinutuzumab (N=216) | Obinutuzumab + Chlorambucil (N=216) |
|---|---|---|
| Progression-free survivala | ||
| Number of events, n (%) | 29 (13) | 79 (37) |
| Disease progression | 14 (6) | 71 (33) |
| Death | 15 (7) | 8 (4) |
| Median, months | Not Reached | Not Reached |
| HR (95% CI)b | 0.33 (0.22, 0.51) | |
| p-valueb | <0.0001 | |
| Response ratec, n (%) | ||
| ORRd | 183 (85) | 154 (71) |
| 95% CI | (79, 89) | (65, 77) |
| CR | 100 (46) | 47 (22) |
| CR+CRid | 107 (50) | 50 (23) |
| PR | 76 (35) | 104 (48) |
CI = confidence interval; CR = complete remission; CRi = complete remission with incomplete marrow recovery; HR = hazard ratio; ORR = overall response rate (CR + CRi + PR); PR = partial remission.
a From randomization until earliest event of disease progression or death due to any cause. IRC-assessed; Kaplan-Meier estimate.
b HR estimate is based on Cox-proportional hazards model stratified by Binet Stage and geographic region; p-value based on log rank test stratified by the same factors.
c Per 2008 International Workshop for Chronic Lymphocytic Leukemia (IWCLL) guidelines.
d p-values based on Cochran-Mantel-Haenszel test; p=0.0007 for ORR; p<0.0001 for CR+CRi.
Figure 1. Kaplan-Meier Curve of IRC-Assessed Progression-free Survival in CLL14:
At the time of analysis, median overall survival (OS) had not been reached, with fewer than 10% of patients experiencing an event. The median duration of follow-up for OS was 28 months.
Minimal residual disease (MRD) was evaluated using allele-specific oligonucleotide polymerase chain reaction (ASO-PCR). The definition of negative status was less than one CLL cell per 104 leukocytes. Rates of MRD negativity 3 months after the completion of treatment regardless of response and in patients who achieved CR are shown in Table 20. At this assessment, 134 patients in the VEN+G arm who were MRD negative in peripheral blood had matched bone marrow specimens; of these, 122 patients (91%) were MRD negative in both peripheral blood and bone marrow.
Table 20. Minimal Residual Disease Negativity Rates Three Months After the Completion of Treatment in CLL14:
| VENCLEXTA + Obinutuzumab | Obinutuzumab + Chlorambucil | |
|---|---|---|
| MRD negativity rate (ITT population) | ||
| N | 216 | 216 |
| Bone marrow, n (%) | 123 (57) | 37 (17) |
| 95% CI | (50, 64) | (12, 23) |
| p-valuea | <0.0001 | |
| Peripheral blood, n (%) | 163 (76) | 76 (35) |
| 95% CI | (69, 81) | (29, 42) |
| p-valuea | <0.0001 | |
| MRD negativity rate in patients with CR | ||
| N | 100 | 47 |
| Bone marrow, n (%) | 69 (69) | 21 (45) |
| 95% CI | (59, 78) | (30, 60) |
| p-valuea | 0.0048 | |
| Peripheral blood, n (%) | 87 (87) | 29 (62) |
| 95% CI | (79, 93) | (46, 75) |
| p-valuea | 0.0005 | |
CI = confidence interval; CR = complete remission.
a p-value based on Chi-square test.
Twelve months after the completion of treatment, MRD negativity rates in peripheral blood were 58% (126/216) in patients treated with VEN+G and 9% (20/216) in patients treated with GClb.
In Combination with Rituximab
MURANO was a randomized (1:1), multicenter, open-label trial (NCT02005471) that evaluated the efficacy and safety of VENCLEXTA in combination with rituximab (VEN+R) versus bendamustine in combination with rituximab (B+R) in patients with CLL who had received at least one line of prior therapy. Patients in the VEN+R arm completed the VENCLEXTA 5-week ramp-up dosing schedule [see Dosage and Administration (2.2, 2.4)] and received VENCLEXTA 400 mg orally once daily for 24 months from Cycle 1 Day 1 of rituximab in the absence of disease progression or unacceptable toxicity. Rituximab was initiated after the 5-week dose ramp-up at a dose of 375 mg/m² intravenously on Day 1 of Cycle 1 and 500 mg/m² intravenously on Day 1 of Cycles 2-6. Patients randomized to B+R received bendamustine 70 mg/m² intravenously on Days 1 and 2 for 6 cycles in combination with rituximab at the above described dose and schedule. Each cycle was 28 days.
A total of 389 patients were randomized: 194 to the VEN+R arm and 195 to the B+R arm. Baseline demographic and disease characteristics were similar between the VEN+R and B+R arms. The median age was 65 years (range: 22 to 85 years), 97% were White, 74% were male, and 99% had ECOG performance status <2. Median prior lines of therapy was 1 (range: 1 to 5); 59% had received 1 prior therapy, 26% had received 2 prior therapies, and 16% had received 3 or more prior therapies. Prior therapies included alkylating agents (94%), anti-CD20 antibodies (77%), B-cell receptor pathway inhibitors (2%), and prior purine analogs (81%, including fludarabine/cyclophosphamide/rituximab in 55%). A 17p deletion was detected in 24% of patients, TP53 mutations in 25%, 11q deletion in 32%, and unmutated IgVH in 63%.
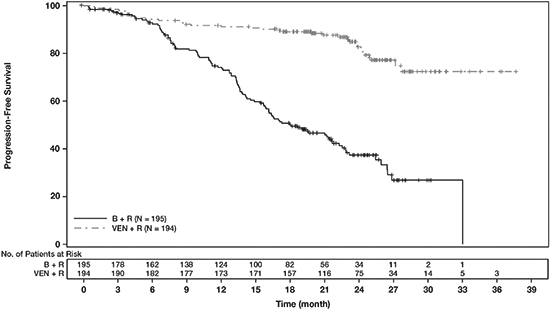
Efficacy was based on PFS as assessed by an IRC. The median follow-up for PFS was 23.4 months (range: 0 to 37.4+ months). Efficacy results for MURANO are shown in Table 21. The Kaplan-Meier curve for PFS is shown in Figure 2.
Table 21. IRC-Assessed Efficacy Results in MURANO:
| Endpoint | VENCLEXTA + Rituximab (N=194) | Bendamustine + Rituximab (N=195) |
|---|---|---|
| Progression-free survivala | ||
| Number of events, n (%) | 35 (18) | 106 (54) |
| Disease progression, n | 26 | 91 |
| Death events, n | 9 | 15 |
| Median, months (95% CI) | Not Reached | 18.1 (15.8, 22.3) |
| HR (95% CI)b | 0.19 (0.13, 0.28) | |
| p-valueb | <0.0001 | |
| Response ratec, n (%) | ||
| ORR | 179 (92) | 141 (72) |
| 95% CI | (88, 96) | (65, 78) |
| CR+CRi | 16 (8) | 7 (4) |
| nPR | 3 (2) | 1 (1) |
| PR | 160 (82) | 133 (68) |
CI = confidence interval; CR = complete remission; CRi = complete remission with incomplete marrow recovery; HR = hazard ratio; nPR = nodular partial remission; ORR = overall response rate (CR + CRi + nPR + PR); PR = partial remission.
a Kaplan-Meier estimate.
a Kaplan-Meier estimate.
b HR estimate is based on Cox-proportional hazards model stratified by 17p deletion, risk status, and geographic region; p-value based on log-rank test stratified by the same factors.
c Per 2008 International Workshop for Chronic Lymphocytic Leukemia (IWCLL) guidelines.
Figure 2. Kaplan-Meier Curve of IRC-Assessed Progression-free Survival in MURANO:
At the time of analysis, median overall survival had not been reached in either arm after a median follow-up of 22.9 months.
At 3 months after the last dose of rituximab, the MRD negativity rate in peripheral blood in patients who achieved PR or better was 53% (103/194) in the VEN+R arm and 12% (23/195) in the B+R arm. The MRD-negative CR/CRi rate at this timepoint was 3% (6/194) in the VEN+R arm and 2% (3/195) in the B+R arm.
Monotherapy
The efficacy of VENCLEXTA monotherapy in previously treated CLL or SLL is based on three single-arm trials.
M13-982
M13-982 (NCT01889186) was an open-label, multicenter trial that enrolled 106 patients with CLL with 17p deletion who had received at least one prior therapy. In the trial, 17p deletion was confirmed in peripheral blood specimens from patients using Vysis CLL FISH Probe Kit, which is FDA approved for selection of patients for VENCLEXTA treatment. Patients received VENCLEXTA 400 mg orally once daily following completion of the ramp-up dosing schedule [see Dosage and Administration (2.2, 2.4)].
Efficacy was based on overall response rate (ORR) as assessed by an IRC.
Table 22 summarizes the baseline demographic and disease characteristics of the trial population.
Table 22. Baseline Patient Characteristics in M13-982:
| Characteristic | N=106 |
|---|---|
| Age, years; median (range) | 67 (37-83) |
| White; % | 97 |
| Male; % | 65 |
| ECOG performance status; % 0 1 2 | 40 52 8 |
| Tumor burden; % Absolute lymphocyte count ≥25 x 109/L One or more nodes ≥5 cm | 50 53 |
| Number of prior therapies; median (range) | 2.5 (1-10) |
| Time since diagnosis, years; median (range)a | 6.6 (0.1-32.1) |
ECOG = Eastern Cooperative Oncology Group.
a N=105.
The median time on treatment at the time of evaluation was 12.1 months (range: 0 to 21.5 months). Efficacy results are shown in Table 23.
Table 23. Efficacy Results per IRC for Patients with Previously Treated CLL with 17p Deletion in M13-982:
| Endpoint | VENCLEXTA N=106 |
|---|---|
| ORR, n (%)a (95% CI) | 85 (80) (71, 87) |
| CR + CRi, n (%) CR, n (%) CRi, n (%) | 8 (8) 6 (6) 2 (2) |
| nPR, n (%) | 3 (3) |
| PR, n (%) | 74 (70) |
CI = confidence interval; CR = complete remission; CRi = complete remission with incomplete marrow recovery; IRC = independent review committee; nPR = nodular partial remission; ORR = overall response rate (CR + CRi + nPR + PR); PR = partial remission.
a Per 2008 IWCLL guidelines.
The median time to first response was 0.8 months (range: 0.1 to 8.1 months).
Based on a later data cutoff date and investigator-assessed efficacy, the duration of response (DOR) ranged from 2.9 to 32.8+ months. The median DOR has not been reached with median follow-up of 22 months.
Minimal residual disease was evaluated in peripheral blood and bone marrow for patients who achieved CR or CRi, following treatment with VENCLEXTA. Three percent (3/106) achieved MRD negativity in the peripheral blood and bone marrow (less than one CLL cell per 104 leukocytes).
M12-175
M12-175 (NCT01328626) was an open-label, multicenter trial that enrolled previously treated patients with CLL or SLL, including those with 17p deletion. Efficacy was evaluated in 67 patients (59 with CLL, 8 with SLL) who had received VENCLEXTA 400 mg orally once daily following completion of a ramp-up dosing schedule. Patients continued this dose until disease progression or unacceptable toxicity. The median duration of treatment at the time of evaluation was 22.1 months (range: 0.5 to 71.7 months).
The median age was 65 years (range: 42 to 84 years), 78% were male and 87% were White. The median number of prior treatments was 3 (range: 1 to 11). At baseline, 67% of patients had one or more nodes ≥5 cm, 30% of patients had ALC ≥25 x 109/L, 33% had documented unmutated IgVH, and 21% had documented 17p deletion.
Efficacy was based on 2008 IWCLL guidelines and assessed by an IRC. The ORR was 76% (95% CI: 64%, 86%), with a CR + CRi rate of 10% and PR rate of 66%. The median DOR was 36.2 months (range: 2.4 to 52.4 months).
M14-032
M14-032 (NCT02141282) was an open-label, multicenter trial that enrolled patients with CLL who had been previously treated with and progressed on or after ibrutinib or idelalisib. Patients received VENCLEXTA 400 mg orally once daily following completion of the ramp-up dosing schedule [see Dosage and Administration (2.2, 2.4)]. Patients continued this dose until disease progression or unacceptable toxicity. At the time of analysis, the median duration of treatment was 19.5 months (range: 0.1 to 39.5 months).
Of the 127 patients treated (91 with prior ibrutinib, 36 with prior idelalisib), the median age was 66 years (range: 28 to 85 years), 70% were male and 92% were White. The median number of prior treatments was 4 (range: 1 to 15). At baseline, 41% of patients had one or more nodes ≥5 cm, 31% had an ALC ≥25 x 109/L, 57% had documented unmutated IgVH, and 39% had documented 17p deletion.
Efficacy was based on 2008 IWCLL guidelines and was assessed by an IRC. The ORR was 70% (95% CI: 61%, 78%), with a CR + CRi rate of 5% and PR rate of 65%. The median DOR was not reached with a median follow-up time of 19.9 months (range: 2.9 to 36 months).
14.2 Acute Myeloid Leukemia
VENCLEXTA was studied in adult patients with newly diagnosed AML who were 75 years or older, or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of 2-3, severe cardiac or pulmonary comorbidity, moderate hepatic impairment, CLcr <45 mL/min, or other comorbidity.
In Combination with Azacitidine or Decitabine
VIALE-A was a randomized (2:1), double-blind, placebo-controlled, multicenter trial (NCT02993523) that evaluated the efficacy and safety of VENCLEXTA in combination with azacitidine (VEN+AZA) versus placebo with azacitidine (PBO+AZA).
Patients received VENCLEXTA 400 mg orally once daily on Days 1-28 following completion of the ramp-up dosing schedule [see Dosage and Administration (2.3)] or placebo in combination with azacitidine 75 mg/m² either intravenously or subcutaneously on Days 1-7 of each 28-day cycle beginning on Cycle 1 Day 1. During the ramp-up, patients received TLS prophylaxis and were hospitalized for monitoring.
Once bone marrow assessment confirmed a remission, defined as less than 5% leukemia blasts with cytopenia following Cycle 1 treatment, VENCLEXTA or placebo was interrupted up to 14 days or until ANC ≥500/microliter and platelet count ≥50 × 103/microliter. For patients with resistant disease at the end of Cycle 1, a bone marrow assessment was performed after Cycle 2 or 3 and as clinically indicated. Azacitidine was resumed on the same day as VENCLEXTA or placebo following interruption. Azacitidine dose reduction was implemented in the clinical trial for management of hematologic toxicity [see Dosage and Administration (2.5)]. Patients continued treatment until disease progression or unacceptable toxicity.
A total of 431 patients were randomized: 286 to the VEN+AZA arm and 145 to the PBO+AZA arm. The baseline demographic and disease characteristic are shown in Table 24.
Table 24. Baseline Demographic and Disease Characteristics in Patients with AML in VIALE-A:
| Characteristic | VENCLEXTA + Azacitidine N=286 | Placebo + Azacitidine N=145 |
|---|---|---|
| Age, years; median (range) | 76 (49, 91) | 76 (60, 90) |
| Race | ||
| White; % | 76 | 75 |
| Black or African American; % | 1 | 1.4 |
| Asian; % | 23 | 23 |
| Males; % | 60 | 60 |
| ECOG performance status; % | ||
| 0-1 | 55 | 56 |
| 2 | 40 | 41 |
| 3 | 5.6 | 3.4 |
| Bone marrow blast; % | ||
| <30% | 30 | 28 |
| ≥30% to <50% | 21 | 23 |
| ≥50% | 49 | 49 |
| Disease history; % | ||
| De Novo AML | 75 | 76 |
| Secondary AML | 25 | 24 |
| Cytogenetic risk detecteda, % | ||
| Intermediate | 64 | 61 |
| Poor | 36 | 39 |
| Mutation analyses detected; n/Nb (%) | ||
| IDH1 or IDH2 | 61/245 (25) | 28/127 (22) |
| IDH1 | 23/245 (9.4) | 11/127 (8.7) |
| IDH2 | 40/245 (16) | 18/127 (14) |
| FLT3 | 29/206 (14) | 22/108 (20) |
| NPM1 | 27/163 (17) | 17/86 (20) |
| TP53 | 38/163 (23) | 14/86 (16) |
a Per the 2016 National Comprehensive Cancer Network (NCCN) Guidelines.
b Number of evaluable BMA specimens received at baseline.
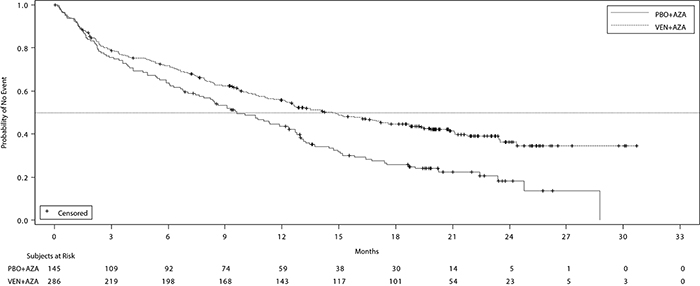
Efficacy was based on overall survival (OS), measured from the date of randomization to death from any cause. The combination of VEN+AZA was superior in OS to PBO+AZA.
The Kaplan-Meier curve for OS is shown in Figure 3. The efficacy results of VIALE-A are shown in Table 25.
Figure 3. Kaplan-Meier Curve for Overall Survival in VIALE-A
Table 25. Efficacy Results in VIALE-A:
| Endpoint | VENCLEXTA + Azacitidine (N=286) | Placebo + Azacitidine (N=145) |
|---|---|---|
| Overall survival | ||
| Mediana, months (95% CI) | 14.7 (11.9, 18.7) | 9.6 (7.4, 12.7) |
| Hazard ratiob (95% CI) | 0.66 (0.52, 0.85) | |
| p-valueb | <0.001 | |
| Response rate | ||
| CR, n (%) | 105 (37) | 26 (18) |
| (95% CI) | (31, 43) | (12, 25) |
| p-valuec | <0.001 | |
| Median DOCRa,d (months) | 18.0 | 13.4 |
| 95% CI | (15.3, -) | (8.7, 17.6) |
| CR+CRh, n (%) | 185 (65) | 33 (23) |
| (95% CI) | (59, 70) | (16, 30) |
| p-valuec | <0.001 | |
| Median DOCR+CRha,e (months) | 17.8 | 13.9 |
| 95% CI | (15.3, -) | (10.4, 15.7) |
CI = confidence interval; CR = complete remission; CRh = complete remission with partial hematologic recovery; DOCR = duration of CR; HR = hazard ratio; - = not reached.
CR (complete remission) was defined as absolute neutrophil count >1,000/microliter, platelets >100,000/microliter, red blood cell transfusion independence, and bone marrow with <5% blasts. Absence of circulating blasts and blasts with Auer rods; absence of extramedullary disease.
CRh (complete remission with partial hematological recovery) was defined as <5% of blasts in the bone marrow, no evidence of disease, and partial recovery of peripheral blood counts (platelets >50,000/microliter and ANC >500/microliter).
a Kaplan-Meier estimate.
b Hazard ratio estimate (VEN+AZA vs. PBO+AZA) is based on Cox-proportional hazards model stratified by cytogenetics (intermediate risk, poor risk) and age (18 to <75, ≥75 years) as assigned at randomization; p-value based on log-rank test stratified by the same factors.
c P-value is from Cochran-Mantel-Haenszel test stratified by age and cytogenetics risk.
d Duration of CR is defined as the number of days from the date of first response of CR to the date of earliest evidence of confirmed morphologic relapse, confirmed progressive disease or death due to disease progression.
e Duration of CR+CRh is defined as the number of days from the date of first response of CR+CRh (the first of either CR or CRh) to the date of earliest evidence of confirmed morphologic relapse, confirmed progressive disease, or death due to disease progression.
Among the patients treated with VEN+AZA, 155 were dependent on red blood cell (RBC) and/or platelets transfusions at baseline; of these patients, 49% (76/155) became independent of RBC and platelet transfusions during any consecutive ≥56-day post-baseline period. Of the patients treated with VEN+AZA, 131 were independent of both RBC and platelet transfusions at baseline, 69% (90/131) remained transfusion independent during any consecutive ≥56-day post-baseline period. Among the patients treated with PBO+AZA, 81 were dependent on RBC and/or platelets transfusions at baseline; of these patients, 27% (22/81) patients became independent of RBC and platelet transfusions during any consecutive ≥56-day post-baseline period. Of the patients treated with PBO+AZA, 64 were independent of both RBC and platelet transfusions at baseline, 42% (27/64) remained transfusion independent during any consecutive ≥56-day post-baseline period.
The median time to first response of CR or CRh was 1.0 months (range: 0.6 to 14.3 months) with VEN+AZA treatment.
M14-358
M14-358 (NCT02203773) was a non-randomized, open-label trial that evaluated the efficacy of VENCLEXTA in combination with azacitidine (N=84) or decitabine (N=31) in patients with newly diagnosed AML. Of those patients, 67 who received azacitidine combination and 13 who received decitabine combination were 75 years or older, or had comorbidities that precluded the use of intensive induction chemotherapy.
Patients received VENCLEXTA 400 mg orally once daily following completion of the ramp-up dosing schedule [see Dosage and Administration (2.3)] in combination with azacitidine (75 mg/m² either intravenously or subcutaneously on Days 1-7 of each 28-day cycle beginning on Cycle 1 Day 1) or decitabine (20 mg/m² intravenously on Days 1-5 of each 28-day cycle beginning on Cycle 1 Day 1). During the ramp-up phase, patients received TLS prophylaxis and were hospitalized for monitoring. Patients continued treatment until disease progression or unacceptable toxicity. Once bone marrow assessment confirmed a remission, defined as less than 5% leukemia blasts, with cytopenia following Cycle 1 treatment, VENCLEXTA was interrupted up to 14 days or until ANC ≥500/microliter and platelet count ≥50 × 103/microliter. Azacitidine dose reduction was implemented in the clinical trial for management of hematologic toxicity [see Dosage and Administration (2.5)]. Dose reductions for decitabine were not implemented in the clinical trial. Baseline demographic and disease characteristic are shown in Table 26.
Table 26. Baseline Patient Characteristics for Patients with AML Treated with VENCLEXTA in Combination with Azacitidine or Decitabine:
| Characteristic | VENCLEXTA + Azacitidine N=67 | VENCLEXTA + Decitabine N=13 |
|---|---|---|
| Age, years; median (range) | 76 (61-90) | 75 (68-86) |
| Race; % | ||
| White | 87 | 77 |
| Black or African American | 4.5 | 0 |
| Asian | 1.5 | 0 |
| Native Hawaiian or Pacific Islander | 1.5 | 15 |
| American Indian/Alaskan Native | 0 | 7.7 |
| Unreported other | 6 | 0 |
| Male; % | 60 | 38 |
| ECOG performance status; % 0-1 2 3 | 64 33 3 | 92 7.7 0 |
| Disease history; % De Novo AML Secondary AML | 73 27 | 85 15 |
| Mutation analyses detecteda; % | ||
| TP53 | 15 | 31 |
| IDH1 or IDH2< | 27 | 0 |
| FLT3 | 16 | 23 |
| NPM1 | 19 | 15 |
| Cytogenetic risk detectedb,c; % | ||
| Intermediate | 64 | 38 |
| Poor | 34 | 62 |
| Baseline comorbiditiesd; % | ||
| Severe cardiac disease | 4.5 | 7.7 |
| Severe pulmonary disease | 1.5 | 0 |
| Moderate hepatic impairment | 9 | 0 |
| Creatinine clearance <45 mL/min | 13 | 7.7 |
ECOG = Eastern Cooperative Oncology Group.
a Includes 6 patients with insufficient sample for analysis in the azacitidine group and 4 in the decitabine group.
b As defined by the National Comprehensive Cancer Network (NCCN) risk categorization v2014.
c No mitosis in 1 patient in azacitidine group (excluded favorable risk by Fluorescence in situ Hybridization [FISH] analysis).
d Patients may have had more than one comorbidity.
The efficacy results are shown in Table 27.
Table 27. Efficacy Results for Patients with Newly Diagnosed AML Treated with VENCLEXTA in Combination with Azacitidine or Decitabine:
| Efficacy Outcomes | VENCLEXTA + Azacitidine N=67 | VENCLEXTA + Decitabine N=13 |
|---|---|---|
| CR, n (%) | 29 (43) | 7 (54) |
| (95% CI) | (31, 56) | (25, 81) |
| CRh, n (%) | 12 (18) | 1 (7.7) |
| (95% CI) | (9.6, 29) | (0.2, 36) |
CI = confidence interval; CR = complete remission; CRh = complete remission with partial hematological recovery.
The median follow-up was 15.9 months (range: 0.4 to 40.3 months) for VENCLEXTA in combination with azacitidine. The median duration of CR was 23.8 months (95% CI: 15.4, -), and the median duration of CR+CRh was 26.5 months (95% CI: 17.4, -).
The median follow-up was 11.0 months (range: 0.7 to 38.8 months) for VENCLEXTA in combination with decitabine. The median duration of CR was 12.7 months (95% CI: 1.4, -) and median duration of CR+CRh was 12.7 months (95% CI: 1.4, 20.0).
Duration of CR is defined as time from the first documentation of CR to the first date of relapse, clinical disease progression or death due to disease progression, whichever occurred earliest. Duration of CR+CRh is defined as time from the first documentation of either CR or CRh to the first date of relapse, clinical disease progression or death due to disease progression, whichever occurred earliest.
Median time to first CR or CRh for patients treated with VENCLEXTA in combination with azacitidine was 1.0 month (range: 0.7 to 8.9 months).
Median time to first CR or CRh for patients treated with VENCLEXTA in combination with decitabine was 1.9 months (range: 0.8 to 4.2 months).
Of patients treated with VENCLEXTA in combination with azacitidine, 12% (8/67) subsequently received stem cell transplant.
The trial enrolled 35 additional patients (age range: 65 to 74 years) who did not have known comorbidities that precluded the use of intensive induction chemotherapy and were treated with VENCLEXTA in combination with azacitidine (N=17) or decitabine (N=18).
For the 17 patients treated with VENCLEXTA in combination with azacitidine, the CR rate was 35% (95% CI: 14%, 62%). The CRh rate was 41% (95% CI: 18%, 67%). Nine (53%) patients subsequently received stem cell transplant.
For the 18 patients treated with VENCLEXTA in combination with decitabine, the CR rate was 56% (95% CI: 31%, 79%). The CRh rate was 22% (95% CI: 6.4%, 48%). Four (22%) patients subsequently received stem cell transplant.
In Combination with Low-Dose Cytarabine
VIALE-C was a randomized (2:1), double-blind, placebo-controlled, multicenter trial (NCT03069352) that evaluated the efficacy and safety of VENCLEXTA in combination with low-dose cytarabine (VEN+LDAC) versus placebo with low-dose cytarabine (PBO+LDAC).
Patients received VENCLEXTA 600 mg orally once daily on Days 1-28 following completion of the ramp-up dosing schedule [see Dosage and Administration (2.3)] or placebo in combination with cytarabine 20 mg/m² subcutaneously once daily on Days 1-10 of each 28-day cycle beginning on Cycle 1 Day 1. During the ramp-up phase, patients received TLS prophylaxis and were hospitalized for monitoring.
Once bone marrow assessment confirmed a remission, defined as less than 5% leukemia blasts with cytopenia following Cycle 1 treatment, VENCLEXTA or placebo was interrupted up to 14 days or until ANC ≥500/microliter and platelet count ≥50 × 103/microliter. For patients with resistant disease at the end of Cycle 1, a bone marrow assessment was performed after Cycle 2 or 3 and as clinically indicated. LDAC was resumed on the same day as VENCLEXTA or placebo following interruption. Patients continued to receive treatment until disease progression or unacceptable toxicity. Baseline demographic and disease characteristic are shown in Table 28.
Table 28. Baseline Demographic and Disease Characteristics in Patients with AML in VIALE-C:
| Characteristic | VENCLEXTA + Low-Dose Cytarabine N=143 | Placebo + Low-Dose Cytarabine N=68 |
|---|---|---|
| Age, years; median (range) | 76 (36, 93) | 76 (41, 88) |
| Race; % | ||
| White | 71 | 69 |
| Black or African American | 1.4 | 1.5 |
| Asian | 27 | 29 |
| Male; % | 55 | 57 |
| ECOG performance status; % 0-1 2 3 | 52 44 4.2 | 50 37 13 |
| Disease history; % De Novo AML Secondary AML | 59 41 | 66 34 |
| Mutation analyses detected; n/Na (%) | ||
| TP53 | 22/112 (20) | 9/52 (17) |
| IDH1 or IDH2 | 21/112 (19) | 12/52 (23) |
| FLT3 | 20/112 (18) | 9/52 (17) |
| NPM1 | 18/112 (16) | 7/52 (13) |
| Cytogenetic risk detectedb; % | ||
| Favorable | <1 | 4 |
| Intermediate | 63 | 63 |
| Poor | 33 | 29 |
a Number of evaluable BMA specimens received at baseline.
b Per the 2016 National Comprehensive Cancer Network (NCCN) Guidelines.
Efficacy was based on the rate of CR and duration of CR with supportive evidence of rate of CR+CRh, duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. The CR rate in the VEN+LDAC arm was 27% (95% CI: 20%, 35%) with a median duration of CR of 11.1 months (95% CI: 6.1, -), and the CR rate in the PBO+LDAC arm was 7.4% (95% CI: 2.4%, 16%) with a median duration of CR of 8.3 months (95% CI: 3.1, -). The CR+CRh rate in the VEN+LDAC arm was 47% (95% CI: 39%, 55%) and in the PBO+LDAC arm was 15% (95% CI: 7.3%, 25%) with a median duration of CR+CRh of 11.1 months with VEN+LDAC treatment and 6.2 months with PBO+LDAC treatment. The median time to first response of CR or CRh was 1.0 month (range: 0.7 to 5.8 months) with VEN+LDAC treatment.
Among the patients treated with VEN+LDAC, 111 were dependent on RBC and/or platelets transfusions at baseline; of these patients, 33% (37/111) patients became independent of RBC and platelet transfusions during any consecutive ≥56-day post-baseline period. Of the patients treated with VEN+LDAC, 32 were independent of both RBC and platelet transfusions at baseline, 50% (16/32) remained transfusion independent during any consecutive ≥56-day post-baseline period.
Among the patients treated with PBO+LDAC, 55 were dependent on RBC and/or platelets transfusions at baseline; of these patients, 13% (7/55) patients became independent of RBC and platelet transfusions during any consecutive ≥56-day post-baseline period. Of the patients treated with PBO+LDAC, 13 were independent of both RBC and platelet transfusions at baseline, 31% (4/13) remained transfusion independent during any consecutive ≥56-day post-baseline period.
VEN+LDAC did not significantly improve OS versus PBO+LDAC. The hazard ratio (HR) for OS was 0.75 (95% CI: 0.52, 1.07); p-value 0.114. The median OS for VEN+LDAC arm was 7.2 months (95% CI: 5.6, 10.1) and for PBO+LDAC arm was 4.1 months (95% CI: 3.1, 8.8).
M14-387
M14-387 (NCT02287233) was a non-randomized, open-label trial that evaluated the efficacy of VEN+LDAC (N=82) in patients with newly diagnosed AML, including patients with previous exposure to a hypomethylating agent for an antecedent hematologic disorder. Of those patients, 61 were 75 years or older, or had comorbidities that precluded the use of intensive induction chemotherapy.
Patients received VENCLEXTA 600 mg orally once daily on Days 1-28 following completion of the ramp-up phase [see Dosage and Administration (2.3)] in combination with cytarabine 20 mg/m² subcutaneously once daily on Days 1-10 of each 28-day cycle beginning on Cycle 1 Day 1. During the ramp-up, patients received TLS prophylaxis and were hospitalized for monitoring. Once bone marrow assessment confirmed a remission, defined as less than 5% leukemia blasts with cytopenia following Cycle 1 treatment, VENCLEXTA was interrupted up to 14 days or until ANC ≥500/microliter and platelet count ≥50 × 103/microliter. Patients continued treatment until disease progression or unacceptable toxicity. Baseline demographic and disease characteristic are shown in Table 29.
Table 29. Baseline Patient Characteristics for Patients with AML Treated with VENCLEXTA in Combination with Low-Dose Cytarabine:
| Characteristic | VENCLEXTA in Combination with Low-Dose Cytarabine N=61 |
|---|---|
| Age, years; median (range) | 76 (63-90) |
| Race; % | |
| White | 92 |
| Black or African American | 1.6 |
| Asian | 1.6 |
| Unreported | 4.9 |
| Male; % | 74 |
| ECOG performance status; % 0-1 2 3 | 66 33 1.6 |
| Disease history; % De Novo AML Secondary AML | 54 46 |
| Mutation analyses detecteda; % | |
| TP53 | 8.2 |
| IDH1 or IDH2 | 23 |
| FLT3 | 21 |
| NPM1 | 9.8 |
| Cytogenetic risk detectedb; % | |
| Intermediate | 59 |
| Poor | 34 |
| No mitoses | 6.6 |
| Baseline comorbiditiesc; % | |
| Severe cardiac disease | 9.8 |
| Moderate hepatic impairment | 4.9 |
| Creatinine clearance ≥30 or <45 mL/min | 3.3 |
a Includes 7 patients with insufficient sample for analysis.
b As defined by the National Comprehensive Cancer Network (NCCN) risk categorization v2014.
c Patients may have had more than one comorbidity.
The median follow-up was 7.3 months (range: 0.3 to 54.0 months). The CR rate was 21% (95% CI: 12, 34) and CRh rate was 21% (95% CI: 12, 34).
The median duration of CR was 22.9 months (95% CI: 5.1, -) and the median duration of CR+CRh was 14.3 months (95% CI: 6.1, 31.2).
Median time to first CR or CRh for patients treated with VEN+LDAC was 1.0 month (range: 0.8 to 9.4 months).
The trial enrolled 21 additional patients (age range: 67 to 74 years) who did not have known comorbidities that precluded the use of intensive induction chemotherapy and were treated with VEN+LDAC. The CR rate was 33% (95% CI: 15%, 57%). The CRh rate was 24% (95% CI: 8.2%, 47%). One patient (4.8%) subsequently received stem cell transplant.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.