ZYLOPRIM Tablet Ref.[27437] Active ingredients: Allopurinol
Source: FDA, National Drug Code (US) Revision Year: 2018
2. Clinical Pharmacology
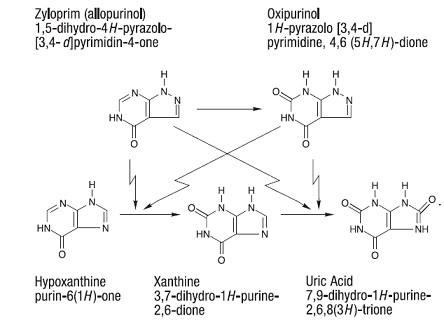
ZYLOPRIM acts on purine catabolism, without disrupting the biosynthesis of purines. It reduces the production of uric acid by inhibiting the biochemical reactions immediately preceding its formation.
ZYLOPRIM is a structural analogue of the natural purine base, hypoxanthine. It is an inhiboitor of xanthine oxidase, the enzyme responsible for the conversion of hypoxanthine to xanthine and of xanthine to uric acid, the end product of purine metabolism in man. ZYLOPRIM is metabolized to the corresponding xanthine analogue, oxipurinol (alloxanthine), which also is an inhibitor of xanthine oxidase.
It has been shown that reutilization of both hypoxanthine and xanthine for nucleotide and nucleic acid synthesis is markedly enhanced when their oxidations are inhibited by ZYLOPRIM and oxipurinol. This reutilization does not disrupt normal nucleic acid anabolism, however, because feedback inhibition is an integral part of purine biosynthesis. As a result of xanthine oxidase inhibition, the serum concentration of hypoxanthine plus xanthine in patients receiving ZYLOPRIM for treatment of hyperuricemia is usually in the range of 0.3 to 0.4 mg/dL compared to a normal level of approximately 0.15 mg/dL. A maximum of 0.9 mg/dL of these oxypurines has been reported when the serum urate was lowered to less than 2 mg/dL by high doses of ZYLOPRIM. These values are far below the saturation levels at which point their precipitation would be expected to occur (above 7 mg/dL).
The renal clearance of hypoxanthine and xanthine is at least 10 times greater than that of uric acid. The increased xanthine and hypoxanthine in the urine have not been accompanied by problems of nephrolithiasis. Xanthine crystalluria has been reported in only three patients. Two of the patients had Lesch-Nyhan syndrome, which is characterized by excessive uric acid production combined with a deficiency of the enzyme, hypoxanthineguanine phosphoribosyltransferase (HGPRTase). This enzyme is required for the conversion of hypoxanthine, xanthine, and guanine to their respective nucleotides. The third patient had lymphosarcoma and produced an extremely large amount of uric acid because of rapid cell lysis during chemotherapy.
ZYLOPRIM is approximately 90% absorbed from the gastrointestinal tract. Peak plasma levels generally occur at 1.5 hours and 4.5 hours for ZYLOPRIM and oxipurinol respectively, and after a single oral dose of 300 mg ZYLOPRIM, maximum plasma levels of about 3 mcg/mL of ZYLOPRIM and 6.5 mcg/mL of oxipurinol are produced.
Approximately 20% of the ingested ZYLOPRIM is excreted in the feces. Because of its rapid oxidation to oxipurinol and a renal clearance rate approximately that of glomerular filtration rate, ZYLOPRIM has a plasma half-life of about 1 to 2 hours. Oxipurinol, however, has a longer plasma half-life (approximately 15 hours) and therefore effective xanthine oxidase inhibition is maintained over a 24-hour period with single daily doses of ZYLOPRIM. Whereas ZYLOPRIM is cleared essentially by glomerular filtration, oxipurinol is reabsorbed in the kidney tubules in a manner similar to the reabsorption of uric acid.
The clearance of oxipurinol is increased by uricosuric drugs, and as a consequence, the addition of a uricosuric agent reduces to some degree the inhibition of xanthine oxidase by oxipurinol and increases to some degree the urinary excretion of uric acid. In practice, the net effect of such combined therapy may be useful in some patients in achieving minimum serum uric acid levels provided the total urinary uric acid load does not exceed the competence of the patient’s renal function.
Hyperuricemia may be primary, as in gout, or secondary to diseases such as acute and chronic leukemia, polycythemia vera, multiple myeloma, and psoriasis. It may occur with the use of diuretic agents, during renal dialysis, in the presence of renal damage, during starvation or reducing diets, and in the treatment of neoplastic disease where rapid resolution of tissue masses may occur. Asymptomatic hyperuricemia is not an indication for treatment with ZYLOPRIM (see INDICATIONS AND USAGE).
Gout is a metabolic disorder which is characterized by hyperuricemia and resultant deposition of monosodium urate in the tissues, particularly the joints and kidneys. The etiology of this hyperuricemia is the overproduction of uric acid in relation to the patient’s ability to excrete it. If progressive deposition of urates is to be arrested or reversed, it is necessary to reduce the serum uric acid level below the saturation point to suppress urate precipitation.
Administration of ZYLOPRIM generally results in a fall in both serum and urinary uric acid within 2 to 3 days. The degree of this decrease can be manipulated almost at will since it is dose-dependent. A week or more of treatment with ZYLOPRIM may be required before its full effects are manifested; likewise, uric acid may return to pretreatment levels slowly (usually after a period of 7 to 10 days following cessation of therapy). This reflects primarily the accumulation and slow clearance of oxipurinol. In some patients a dramatic fall in urinary uric acid excretion may not occur, particularly in those with severe tophaceous gout. It has been postulated that this may be due to the mobilization of urate from tissue deposits as the serum uric acid level begins to fall.
The action of ZYLOPRIM differs from that of uricosuric agents, which lower the serum uric acid level by increasing urinary excretion of uric acid. ZYLOPRIM reduces both the serum and urinary uric acid levels by inhibiting the formation of uric acid. The use of ZYLOPRIM to block the formation of urates avoids the hazard of increased renal excretion of uric acid posed by uricosuric drugs.
ZYLOPRIM can substantially reduce serum and urinary uric acid levels in previously refractory patients even in the presence of renal damage serious enough to render uricosuric drugs virtually ineffective. Salicylates may be given conjointly for their antirheumatic effect without compromising the action of ZYLOPRIM. This is in contrast to the nullifying effect of salicylates on uricosuric drugs.
ZYLOPRIM also inhibits the enzymatic oxidation of mercaptopurine, the sulfur-containing analogue of hypoxanthine, to 6-thiouric acid. This oxidation, which is catalyzed by xanthine oxidase, inactivates mercaptopurine. Hence, the inhibition of such oxidation by ZYLOPRIM may result in as much as a 75% reduction in the therapeutic dose requirement of mercaptopurine when the two compounds are given together.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.