Insulin icodec
Mechanism of action
A slow and steady glucose-lowering effect of insulin icodec is driven by albumin binding as well as reduced insulin receptor binding and clearance. The extended half-life of insulin icodec reflects a depot of insulin icodec in the circulation and in the interstitial compartment, from which insulin icodec is slowly and continuously released and binds specifically to the insulin receptor. When insulin icodec binds to the human insulin receptor it results in the same pharmacological effects as human insulin.
The primary action of insulin, including insulin icodec, is to regulate glucose metabolism. Insulin and its analogues lower blood glucose by activating specific insulin receptors to stimulate peripheral glucose uptake, especially by skeletal muscle and fat as well as to inhibit hepatic glucose production. Insulin also inhibits lipolysis and proteolysis and enhances protein synthesis.
Pharmacodynamic properties
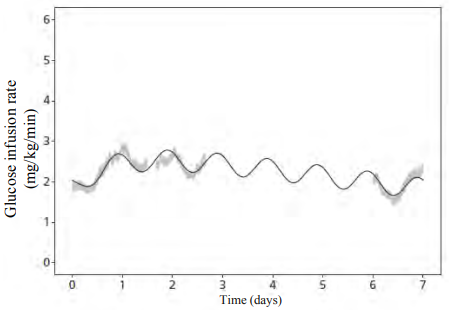
The steady-state pharmacodynamic properties of insulin icodec were investigated in a trial with type 2 diabetes patients. The partial pharmacodynamic properties of insulin icodec were measured in 3 euglycaemic clamps (6.7 mmol/L) during steady state covering 3.5 of the 7 days dosing interval. Glucose infusion rate (GIR) profiles for all three clamps are shown in together with the model-derived data, suggesting the duration of the glucose-lowering effect to cover a full week (Figure 1).
Figure 1. Full-week glucose infusion rate profile of insulin icodec at steady-state in type 2 diabetes:
Notes: Shaded areas are standard error of the mean of individual glucose infusion rate (GIR) profiles (pooled across three steady-state weeks). Line is mean of individual model-predicted GIR profiles (for one steady-state week).
Based on data where insulin icodec was injected at 20:00 (corresponding to day 0).
Clinical steady state was reached after 2-4 weeks when initiating insulin icodec without a one-time additional dose and after 2-3 weeks when initiating insulin icodec with a one-time additional dose of 50% with the first dose.
Pharmacokinetic properties
Overall, pharmacokinetic (PK) properties were similar between groups assessed by population-PK analysis in confirmatory trials, with a trend towards higher exposure with higher anti-drug antibodies (ADA) titres. The effect is not considered clinically relevant as the relative exposure (Cavg) was inside the 0.8-1.25 interval when compared to ADA-negative subjects. Overall ADA prevalence was 70-82%.
Absorption
Insulin icodec is a basal insulin that binds reversibly to albumin, resulting in a slow release of insulin icodec from the essentially inactive depot in circulation and interstitial compartment.
After subcutaneous injection, clinical steady state was reached after 2-4 weeks when initiating insulin icodec without a one-time additional dose and after 2-3 weeks when initiating insulin icodec with a one-time additional dose of 50% with the first dose.
After subcutaneous injection of insulin icodec, the week-to-week intra-subject variability in total exposure is considered low (coefficient of variation for insulin icodec at steady state was 5.90% in type 2 diabetes patients).
Distribution
The affinity of insulin icodec to serum albumin corresponds to a plasma protein binding of >99% in human plasma. No clinically relevant differences in pharmacokinetics properties of insulin icodec are seen across serum albumin levels.
The results of the in vitro protein binding studies demonstrate that there is no clinically relevant interaction between insulin icodec and fatty acids or other protein-bound medicinal products.
Biotransformation
Degradation of insulin icodec is similar to that of human insulin; all metabolites formed are inactive.
Elimination
The half-life after subcutaneous administration is approximately one week independent of dose.
Linearity
Dose proportionality in total exposure is observed after subcutaneous administration within the therapeutic dose range.
Sex, elderly, renal and hepatic impairment
Overall, the pharmacokinetic properties of insulin icodec were preserved and there was no clinically relevant difference in exposure between female and male subjects, between elderly and younger adult subjects (range of studied age of 18-86 years old), or between healthy subjects and subjects with renal or hepatic impairment.
Preclinical safety data
The ratio of mitogenic relative to metabolic potency for insulin icodec is comparable to that of human insulin.
Non-clinical data reveal no special safety concerns for humans based on studies of safety pharmacology, repeated dose toxicity, and toxicity to reproduction.
Related medicines
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.