Mecasermin
Interactions
Mecasermin interacts in the following cases:
Hypoglycaemic medicinal products
Doses of insulin and/or other hypoglycaemic medicinal products may need to be reduced.
Lymphoid tissue hypertrophy
Lymphoid tissue (e.g., tonsillar) hypertrophy associated with complications, such as snoring, sleep apnoea, and chronic middle-ear effusions have been reported with the use of this medicinal product. Patients should have examinations periodically and at the occurrence of clinical symptoms to rule out such potential complications or to initiate appropriate treatment.
Slipped capital femoral epiphysis
Slipped capital femoral epiphysis (with the potential to lead to avascular necrosis) and progression of scoliosis can occur in patients who experience rapid growth. These conditions and other symptoms and signs known to be associated with GH treatment in general should be monitored during mecasermin treatment. Any patient with the onset of a limp or complaint of hip or knee pain should be evaluated.
Hypersensitivity, urticaria, pruritus, erythema
In post-marketing experience in patients treated with mecasermin, cases of hypersensitivity, urticaria, pruritus and erythema have been reported. These have been observed both as being systemic and/or local to the injection site. A small number of cases indicative of anaphylaxis requiring hospitalisation have been reported. Parents and patients should be informed that such reactions are possible and that if a systemic allergic reaction occurs, treatment should be interrupted and prompt medical attention should be sought.
Intracranial hypertension (IH)
Intracranial hypertension (IH) with papilloedema, visual changes, headache, nausea and/or vomiting has been reported in patients treated with mecasermin, as has been reported with therapeutic GH administration. IH-associated signs and symptoms resolved after interruption of dosing. Funduscopic examination is recommended at the initiation, periodically during the course of mecasermin therapy and at the occurrence of clinical symptoms.
Pregnancy
There are no or limited amount of data for the use of mecasermin in pregnant women. Animal studies are insufficient with respect to reproductive toxicity. The potential risk for humans is unknown. This medicinal product should not be used during pregnancy unless clearly necessary.
Nursing mothers
Breast-feeding while taking mecasermin is not recommended, because there is insufficient information on the excretion of mecasermin in human milk.
Carcinogenesis, mutagenesis and fertility
Women of childbearing potential / Contraception in males and females
A negative pregnancy test is recommended for all women of child bearing potential prior to treatment with mecasermin. It is also recommended that all women of childbearing potential use adequate contraception during treatment.
Fertility
Mecasermin has been tested in a rat teratology study with no effects on fœtus up to 16 mg/kg (20 fold the maximum recommended human dose (MRHD) based on body surface area) and in a rabbit teratology with no effects on foetus at dose of 0.5 mg/kg (2 fold the MRHD based on body surface area). Mecasermin has no effects on fertility in rats using intravenous doses 0.25, 1, and 4 mg/day (up to 4 times the clinical exposure with the MRHD based on AUC).
The effects of mecasermin on the unborn child have not been studied. Therefore there is insufficient medical information to determine whether there are significant risks to a foetus. Studies have not been conducted with mecasermin in breast-feeding mothers. Mecasermin should not be given to pregnant or nursing women. A negative pregnancy test and adequate contraception is required in all pre-menopausal women receiving mecasermin.
Effects on ability to drive and use machines
Mecasermin may have a major influence on the ability to drive or use machines in case of a hypoglycaemic episode. Hypoglycaemia is a very common adverse reaction.
Adverse reactions
Summary of the safety profile
Adverse reaction data was taken from a total of 413 clinical trial patients with severe Primary IGFD. Data was also collected from post-marketing sources.
The most frequently reported adverse reactions from the clinical trials were headache (44%), hypoglycaemia (28%), vomiting (26%), injection site hypertrophy (17%), and otitis media (17%).
Intracranial hypertension/increased intracranial pressure occurred in 4 (0.96%) of patients from the clinical trials and occurred in 7–9 year old treatment naïve subjects.
During clinical trials in other indications totaling approximately 300 patients, reports of local and/or systemic hypersensitivity were received for 8% of patients. There were also reports of systemic hypersensitivity from post-marketing use, of which some cases were indicative of anaphylaxis. Post-marketing reports of local allergic reactions were also received.
Some patients may develop antibodies to mecasermin. No attenuation of growth was observed as a consequence of the development of antibodies.
List of adverse reactions
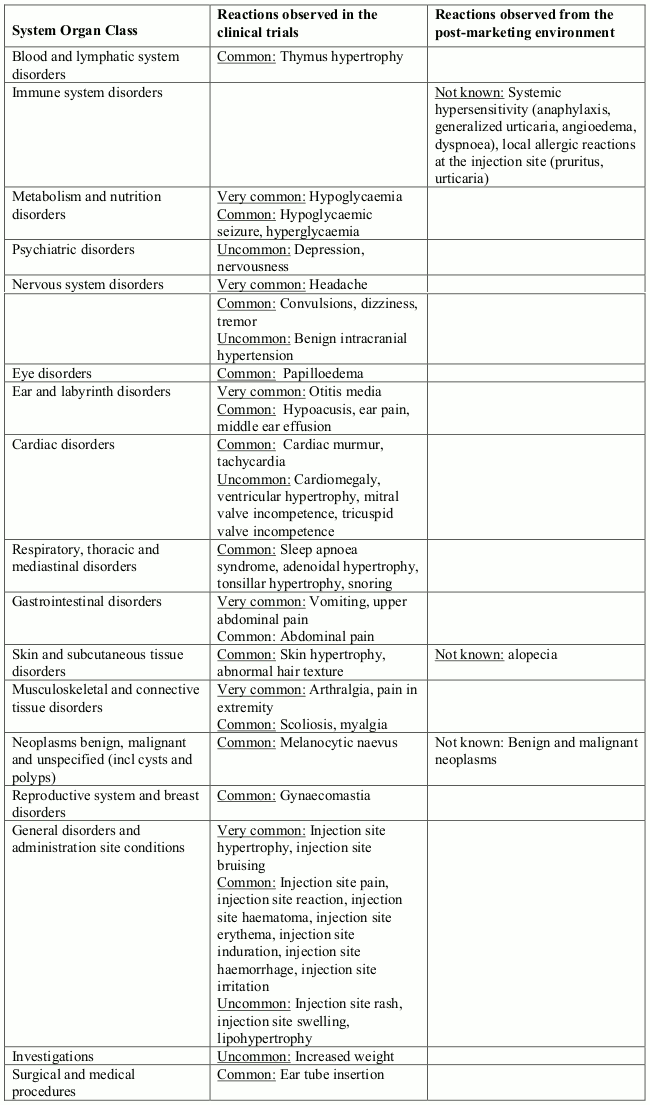
The following list contains very common (≥1/10), common (≥1/100 to <1/10) and uncommon (≥1/1000, <1/100) adverse reactions which occurred in clinical trials. Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. Other adverse reactions have been identified during post approval use of mecasermin. As these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency (not known).
Adverse reactions:
Description of selected adverse reactions
Neoplasms
There have been post-marketing reports of benign and malignant neoplasms in children and adolescents who have received treatment with mecasermin. These cases represented a variety of different malignancies and included rare malignancies usually not seen in children.
Systemic/local hypersensitivity
Clinical Trial
During clinical trials in other indications (totaling approximately 300 patients) 8% of patients reported a local and/or systemic hypersensitivity reactions. All cases were mild or moderate in severity and none was serious.
Post-marketing reports
Systemic hypersensitivity included symptoms such as anaphylaxis, generalized urticaria, angioedema and dyspnoea. The symptoms in the cases indicative of anaphylaxis included hives, angioedema and dyspnoea. Some patients required hospitalization. Upon re-administration, symptoms did not re-occur in all patients. There were also reports of local allergic reactions at the injection site. Typically these were pruritus and urticaria.
Hypoglycaemia
Of the 115 (28%) subjects who experienced one or more episode of hypoglycaemia, 6 subjects experienced a hypoglycaemic seizure on one or more occasion. Symptomatic hypoglycaemia was generally avoided when a meal or snack was consumed either shortly before or after the administration of mecasermin.
Injection site hypertrophy
This reaction occurred in 71 (17%) subjects from the clinical trials and was generally associated with lack of proper rotation of injections. When injections were properly dispersed, the condition resolved.
Tonsillar hypertrophy
This was noted in 38 (9%) subjects, particularly in the first 1 to 2 years of therapy with lesser tonsillar growth in subsequent years.
Snoring
This occurred generally in the first year of treatment and was reported in 30 subjects (7%).
Intracranial hypertension/increased intracranial pressure
This occurred in 4 subjects (0.96%); in two subjects mecasermin was discontinued and not restarted; in two subjects the event did not recur after restarting mecasermin at a reduced dose. All 4 subjects recovered from the event without sequelae.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.