HERCESSI Solution for injection Ref.[109764] Active ingredients: Trastuzumab
Source: FDA, National Drug Code (US) Revision Year: 2024
4. Contraindications
None.
5. Warnings and Precautions
5.1 Cardiomyopathy
Trastuzumab products can cause left ventricular cardiac dysfunction, arrhythmias, hypertension, disabling cardiac failure, cardiomyopathy, and cardiac death [see Boxed Warning: Cardiomyopathy]. Trastuzumab products can also cause asymptomatic decline in left ventricular ejection fraction (LVEF).
There is a 4-6 fold increase in the incidence of symptomatic myocardial dysfunction among patients receiving trastuzumab products as a single agent or in combination therapy compared with those not receiving trastuzumab products. The highest absolute incidence occurs when trastuzumab product is administered with ananthracycline.
Withhold Hercessi for ≥16% absolute decrease in LVEF from pre-treatment values or an LVEF value below institutional limits of normal and ≥ 10% absolute decrease in LVEF from pretreatment values [see Dosage and Administration (2.3)]. The safety of continuation or resumption of Hercessi in patients with trastuzumab product-induced left ventricular cardiac dysfunction has not been studied.
Patients who receive anthracycline after stopping Hercessi may also be at increased risk of cardiac dysfunction [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
Cardiac Monitoring
Conduct thorough cardiac assessment, including history, physical examination, and determination of LVEF by echocardiogram or MUGA scan. The following schedule is recommended:
- Baseline LVEF measurement immediately prior to initiation of Hercessi
- LVEF measurements every 3 months during and upon completion of Hercessi
- Repeat LVEF measurement at 4 week intervals if Hercessi is withheld for significant left ventricular cardiac dysfunction [see Dosage and Administration (2.3)]
- LVEF measurements every 6 months for at least 2 years following completion of Hercessi as a component of adjuvant therapy.
In Study 1, 15% (158/1031) of patients discontinued trastuzumab due to clinical evidence of myocardial dysfunction or significant decline in LVEF after a median follow-up duration of 8.7 years in the AC-TH (anthracycline, cyclophosphamide, paclitaxel, and trastuzumab) arm. In Study 3 (one-year trastuzumab treatment), the number of patients who discontinued trastuzumab due to cardiac toxicity at 12.6 months median duration of follow-up was 2.6% (44/1678). In Study 4, a total of 2.9% (31/1056) of patients in the TCH (docetaxel, carboplatin, trastuzumab) arm (1.5% during the chemotherapy phase and 1.4% during the monotherapy phase) and 5.7% (61/1068) of patients in the AC-TH arm (1.5% during the chemotherapy phase and 4.2% during the monotherapy phase) discontinued trastuzumab due to cardiac toxicity.
Among 64 patients receiving adjuvant chemotherapy (Studies 1 and 2) who developed congestive heart failure, one patient died of cardiomyopathy, one patient died suddenly without documented etiology, and 33 patients were receiving cardiac medication at last follow-up. Approximately 24% of the surviving patients had recovery to a normal LVEF (defined as ≥ 50%) and no symptoms on continuing medical management at the time of last follow-up. Incidence of congestive heart failure (CHF) is presented in Table 1. The safety of continuation or resumption of Hercessi in patients with trastuzumab product-induced left ventricular cardiac dysfunction has not been studied.
Table 1. Incidence of Congestive Heart Failure in Adjuvant Breast Cancer Studies:
| Study | Regimen | Incidence of CHF | |
|---|---|---|---|
| Trastuzumab | Control | ||
| 1 & 2^a^ | AC^b^ → Paclitaxel + Trastuzumab | 3.2% (64/2000)c | 1.3% (21/1655) |
| 3^d^ | Chemo → Trastuzumab | 2% (30/1678) | 0.3% (5/1708) |
| 4 | ACb → Docetaxel + Trastuzumab | 2% (20/1068) | 0.3% (3/1050) |
| 4 | Docetaxel + Carbo + Trastuzumab | 0.4% (4/1056) | 0.3% (3/1050) |
a Median follow-up duration for studies 1 and 2 combined was 8.3 years in the AC→TH arm.
b Anthracycline (doxorubicin) and cyclophosphamide.
c Includes 1 patient with fatal cardiomyopathy and 1 patient with sudden death without documented etiology.
d Includes NYHA II-IV and cardiac death at 12.6 months median duration of follow-up in the one-year trastuzumab arm.
In Study 3 (one-year trastuzumab treatment), at a median follow-up duration of 8 years, the incidence of severe CHF (NYHA III & IV) was 0.8%, and the rate of mild symptomatic and asymptomatic left ventricular dysfunction was 4.6%.
Table 2. Incidence of Cardiac Dysfunctiona in Metastatic Breast Cancer Studies:
| Study | Event | Incidence | |||
|---|---|---|---|---|---|
| NYHA I-IV | NYHA III-IV | ||||
| Trastuzumab | Control | Trastuzumab | Control | ||
| 5 (AC)b | Cardiac Dysfunction | 28% | 7% | 19% | 3% |
| 5 (paclitaxel) | Cardiac Dysfunction | 11% | 1% | 4% | 1% |
| 6 | Cardiac Dysfunction^c^ | 7% | N/A | 5% | N/A |
a Congestive heart failure or significant asymptomatic decrease in LVEF.
b Anthracycline (doxorubicin or epirubicin) and cyclophosphamide.
c Includes 1 patient with fatal cardiomyopathy.
In Study 4, the incidence of NCI-CTC Grade ¾ cardiac ischemia/infarction was higher in the trastuzumab containing regimens (AC-TH: 0.3% (3/1068) and TCH: 0.2% (2/1056)) as compared to none in AC-T.
5.2 Infusion Reactions
Infusion reactions consist of a symptom complex characterized by fever and chills, and on occasion included nausea, vomiting, pain (in some cases at tumor sites), headache, dizziness, dyspnea, hypotension, rash, and asthenia [see Adverse Reactions (6.1)].
In post-marketing reports, serious and fatal infusion reactions have been reported. Severe reactions, which include bronchospasm, anaphylaxis, angioedema, hypoxia, and severe hypotension were usually reported during or immediately following the initial infusion. However, the onset and clinical course were variable, including progressive worsening, initial improvement followed by clinical deterioration, or delayed postinfusion events with rapid clinical deterioration. For fatal events, death occurred within hours to days following a serious infusion reaction.
Interrupt Hercessi infusion in all patients experiencing dyspnea, clinically significant hypotension, and intervention of medical therapy administered (which may include epinephrine, corticosteroids, diphenhydramine, bronchodilators, and oxygen). Patients should be evaluated and carefully monitored until complete resolution of signs and symptoms. Permanent discontinuation should be strongly considered in all patients with severe infusion reactions.
There are no data regarding the most appropriate method of identification of patients who may safely be retreated with trastuzumab products after experiencing a severe infusion reaction. Prior to resumption of trastuzumab infusion, the majority of patients who experienced a severe infusion reaction were premedicated with antihistamines and/or corticosteroids. While some patients tolerated Trastuzumab infusions, others had recurrent severe infusion reactions despite pre-medications.
5.3 Embryo-Fetal Toxicity
Trastuzumab products can cause fetal harm when administered to a pregnant woman. In post-marketing reports, use of trastuzumab during pregnancy resulted in cases of oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death.
Verify the pregnancy status of females of reproductive potential prior to the initiation of Hercessi. Advise pregnant women and females of reproductive potential that exposure to Hercessi during pregnancy or within 7 months prior to conception can result in fetal harm. Advise females of reproductive potential to use effective contraception during treatment and for 7 months following the last dose of Hercessi [see Use in Specific Populations (8.1, 8.3) and Clinical Pharmacology (12.3)].
5.4 Pulmonary Toxicity
Trastuzumab product use can result in serious and fatal pulmonary toxicity. Pulmonary toxicity includes dyspnea, interstitial pneumonitis, pulmonary infiltrates, pleural effusions, non-cardiogenic pulmonary edema, pulmonary insufficiency and hypoxia, acute respiratory distress syndrome, and pulmonary fibrosis. Such events can occur as sequelae of infusion reactions [see Warnings and Precautions (5.2)]. Patients with symptomatic intrinsic lung disease or with extensive tumor involvement of the lungs, resulting in dyspnea at rest, appear to have more severe toxicity.
5.5 Exacerbation of Chemotherapy-Induced Neutropenia
In randomized, controlled clinical trials, the per-patient incidences of NCI-CTC Grade 3−4 neutropenia and of febrile neutropenia were higher in patients receiving trastuzumab in combination with myelosuppressive chemotherapy as compared to those who received chemotherapy alone. The incidence of septic death was similar among patients who received trastuzumab and those who did not [see Adverse Reactions (6.1)].
6. Adverse Reactions
The following adverse reactions are discussed in greater detail in other sections of the label:
- Cardiomyopathy [see Warnings and Precautions (5.1)]
- Infusion Reactions [see Warnings and Precautions (5.2)]
- Embryo-Fetal Toxicity [see Warnings and Precautions (5.3)]
- Pulmonary Toxicity [see Warnings and Precautions (5.4)]
- Exacerbation of Chemotherapy-Induced Neutropenia [see Warnings and Precautions (5.5)]
The most common adverse reactions in patients receiving trastuzumab products in the adjuvant and metastatic breast cancer setting are fever, nausea, vomiting, infusion reactions, diarrhea, infections, increased cough, headache, fatigue, dyspnea, rash, neutropenia, anemia, and myalgia. Adverse reactions requiring interruption or discontinuation of trastuzumab product treatment include CHF, significant decline in left ventricular cardiac function, severe infusion reactions, and pulmonary toxicity [see Dosage and Administration (2.3)].
In the metastatic gastric cancer setting, the most common adverse reactions (≥ 10%) that were increased (≥ 5% difference) in the patients receiving trastuzumab as compared to patients receiving chemotherapy alone were neutropenia, diarrhea, fatigue, anemia, stomatitis, weight loss, upper respiratory tract infections, fever, thrombocytopenia, mucosal inflammation, nasopharyngitis, and dysgeusia. The most common adverse reactions which resulted in discontinuation of trastuzumab treatment in the absence of disease progression were infection, diarrhea, and febrile neutropenia.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adjuvant Breast Cancer Studies
The data below reflect exposure to one-year trastuzumab therapy across three randomized, open-label studies, Studies 1, 2, and 3, with (n = 3678) or without (n = 3363) trastuzumab in the adjuvant treatment of breast cancer.
The data summarized in Table 3 below, from Study 3, reflect exposure to trastuzumab in 1678 patients; the median treatment duration was 51 weeks and median number of infusions was 18. Among the 3386 patients enrolled in the observation and one-year trastuzumab arms of Study 3 at a median duration of follow-up of 12.6 months in the trastuzumab arm, the median age was 49 years (range: 21 to 80 years), 83% of patients were Caucasian, and 13% were Asian.
Table 3. Adverse Reactions for Study 3a, All Gradesb:
| Adverse Reaction | One Year Trastuzumab (n = 1678) | Observation (n = 1708) |
|---|---|---|
| Cardiac | ||
| Hypertension | 64 (4%) | 35 (2%) |
| Dizziness | 60 (4%) | 29 (2%) |
| Ejection Fraction Decreased | 58 (3.5%) | 11 (0.6%) |
| Palpitations | 48 (3%) | 12 (0.7%) |
| Cardiac Arrhythmiasc | 40 (3%) | 17 (1%) |
| Cardiac Failure Congestive | 30 (2%) | 5 (0.3%) |
| Cardiac Failure | 9 (0.5%) | 4 (0.2%) |
| Cardiac Disorder | 5 (0.3%) | 0 (0%) |
| Ventricular Dysfunction | 4 (0.2%) | 0 (0%) |
| Respiratory Thoracic Mediastinal Disorders | ||
| Cough | 81 (5%) | 34 (2%) |
| Influenza | 70 (4%) | 9 (0.5%) |
| Dyspnea | 57 (3%) | 26 (2%) |
| URI | 46 (3%) | 20 (1%) |
| Rhinitis | 36 (2%) | 6 (0.4%) |
| Pharyngolaryngeal pain | 32 (2%) | 8 (0.5%) |
| Sinusitis | 26 (2%) | 5 (0.3%) |
| Epistaxis | 25 (2%) | 1 (0.06%) |
| Pulmonary Hypertension | 4 (0.2%) | 0 (0%) |
| Interstitial Pneumonitis | 4 (0.2%) | 0 (0%) |
| Gastrointestinal Disorders | ||
| Diarrhea | 123 (7%) | 16 (1%) |
| Nausea | 108 (6%) | 19 (1%) |
| Vomiting | 58 (3.5%) | 10 (0.6%) |
| Constipation | 33 (2%) | 17 (1%) |
| Dyspepsia | 30 (2%) | 9 (0.5%) |
| Upper Abdominal Pain | 29 (2%) | 15 (1%) |
| Musculoskeletal & Connective Tissue Disorders | ||
| Arthralgia | 137 (8%) | 98 (6%) |
| Back Pain | 91 (5%) | 58 (3%) |
| Myalgia | 63 (4%) | 17 (1%) |
| Bone Pain | 49 (3%) | 26 (2%) |
| Muscle Spasm | 46 (3%) | 3 (0.2%) |
| Nervous System Disorders | ||
| Headache | 162 (10%) | 49 (3%) |
| Paraesthesia | 29 (2%) | 11 (0.6%) |
| Skin & Subcutaneous Tissue Disorders | ||
| Rash | 70 (4%) | 10 (0.6%) |
| Nail Disorders | 43 (2%) | 0 (0%) |
| Pruritus | 40 (2%) | 10 (0.6%) |
| General Disorders | ||
| Pyrexia | 100 (6%) | 6 (0.4%) |
| Edema Peripheral | 79 (5%) | 37 (2%) |
| Chills | 85 (5%) | 0 (0%) |
| Asthenia | 75 (4.5%) | 30 (2%) |
| Influenza-like Illness | 40 (2%) | 3 (0.2%) |
| Sudden Death | 1 (0.06%) | 0 (0%) |
| Infections | ||
| Nasopharyngitis | 135 (8%) | 43 (3%) |
| UTI | 39 (3%) | 13 (0.8%) |
| Immune System Disorders | ||
| Hypersensitivity | 10 (0.6%) | 1 (0.06%) |
| Autoimmune Thyroiditis | 4 (0.3%) | 0 (0%) |
a Median follow-up duration of 12.6 months in the one-year trastuzumab treatment arm.
b The incidence of Grade 3 or higher adverse reactions was < 1% in both arms for each listed term.
c Higher level grouping term.
In Study 3, a comparison of 3-weekly trastuzumab treatment for two years versus one year was also performed. The rate of asymptomatic cardiac dysfunction was increased in the 2-year trastuzumab treatment arm (8.1% versus 4.6% in the one-year trastuzumab treatment arm). More patients experienced at least one adverse reaction of Grade 3 or higher in the 2-year trastuzumab treatment arm (20.4%) compared with the one-year trastuzumab treatment arm (16.3%).
The safety data from Studies 1 and 2 were obtained from 3655 patients, of whom 2000 received trastuzumab; the median treatment duration was 51 weeks. The median age was 49 years (range: 24−80); 84% of patients were White, 7% Black, 4% Hispanic, and 3% Asian.
In Study 1, only Grade 3 – 5 adverse events, treatment-related Grade 2 events, and Grade 2 – 5 dyspnea were collected during and for up to 3 months following protocol-specified treatment. The following non-cardiac adverse reactions of Grade 2 – 5 occurred at an incidence of at least 2% greater among patients receiving trastuzumab plus chemotherapy as compared to chemotherapy alone: fatigue (29.5% vs. 22.4%), infection (24.0% vs. 12.8%), hot flashes (17.1% vs. 15.0%), anemia (12.3% vs. 6.7%), dyspnea (11.8% vs. 4.6%), rash/desquamation (10.9% vs. 7.6%), leukopenia (10.5% vs. 8.4%), neutropenia (6.4% vs. 4.3%), headache (6.2% vs. 3.8%), pain (5.5% vs. 3.0%), edema (4.7% vs. 2.7%), and insomnia (4.3% vs. 1.5%). The majority of these events were Grade 2 in severity.
In Study 2, data collection was limited to the following investigator-attributed treatment-related adverse reactions: NCI-CTC Grade 4 and 5 hematologic toxicities, Grade 3 – 5 non-hematologic toxicities, selected Grade 2 – 5 toxicities associated with taxanes (myalgia, arthralgias, nail changes, motor neuropathy, and sensory neuropathy) and Grade 1 – 5 cardiac toxicities occurring during chemotherapy and/or trastuzumab treatment. The following non-cardiac adverse reactions of Grade 2 – 5 occurred at an incidence of at least 2% greater among patients receiving trastuzumab plus chemotherapy as compared to chemotherapy alone: arthralgia (12.2% vs. 9.1%), nail changes (11.5% vs. 6.8%), dyspnea (2.4% vs. 0.2%), and diarrhea (2.2% vs. 0%). The majority of these events were Grade 2 in severity.
Safety data from Study 4 reflect exposure to trastuzumab as part of an adjuvant treatment regimen from 2124 patients receiving at least one dose of study treatment [AC-TH: n = 1068; TCH: n =1056]. The overall median treatment duration was 54 weeks in both the AC-TH and TCH arms. The median number of infusions was 26 in the AC-TH arm and 30 in the TCH arm, including weekly infusions during the chemotherapy phase and every three week dosing in the monotherapy period. Among these patients, the median age was 49 years (range 22 to 74 years). In Study 4, the toxicity profile was similar to that reported in Studies 1, 2, and 3 with the exception of a low incidence of CHF in the TCH arm.
Metastatic Breast Cancer Studies
The data below reflect exposure to trastuzumab in one randomized, open-label study, Study 5, of chemotherapy with (n = 235) or without (n = 234) trastuzumab in patients with metastatic breast cancer, and one single-arm study (Study 6; n = 222) in patients with metastatic breast cancer. Data in Table 4 are based on Studies 5 and 6.
Among the 464 patients treated in Study 5, the median age was 52 years (range: 25−77 years). Eighty-nine percent were White, 5% Black, 1% Asian, and 5% other racial/ethnic groups. All patients received 4 mg/kg initial dose of trastuzumab followed by 2 mg/kg weekly. The percentages of patients who received trastuzumab treatment for ≥ 6 months and ≥ 12 months were 58% and 9%, respectively.
Among the 352 patients treated in single agent studies (213 patients from Study 6), the median age was 50 years (range 28 – 86 years), 86% were White, 3% were Black, 3% were Asian, and 8% in other racial/ethnic groups. Most of the patients received 4 mg/kg initial dose of trastuzumab followed by 2 mg/kg weekly. The percentages of patients who received trastuzumab treatment for ≥ 6 months and ≥ 12 months were 31% and 16%, respectively.
Table 4. Per-Patient Incidence of Adverse Reactions Occurring in ≥ 5% of Patients in Uncontrolled Studies or at Increased Incidence in the Trastuzumab Arm (Studies 5 and 6):
| Single Agenta n = 352 | Trastuzumab + Paclitaxel n = 91 | Paclitaxel Alone n = 95 | Trastuzumab + ACb n = 143 | ACb Alone n = 135 | |
|---|---|---|---|---|---|
| Body as a Whole | |||||
| Pain | 47% | 61% | 62% | 57% | 42% |
| Asthenia | 42% | 62% | 57% | 54% | 55% |
| Fever | 36% | 49% | 23% | 56% | 34% |
| Chills | 32% | 41% | 4% | 35% | 11% |
| Headache | 26% | 36% | 28% | 44% | 31% |
| Abdominal pain | 22% | 34% | 22% | 23% | 18% |
| Back pain | 22% | 34% | 30% | 27% | 15% |
| Infection | 20% | 47% | 27% | 47% | 31% |
| Flu syndrome | 10% | 12% | 5% | 12% | 6% |
| Accidental injury | 6% | 13% | 3% | 9% | 4% |
| Allergic reaction | 3% | 8% | 2% | 4% | 2% |
| Cardiovascular | |||||
| Tachycardia | 5% | 12% | 4% | 10% | 5% |
| Congestive heart failure | 7% | 11% | 1% | 28% | 7% |
| Digestive | |||||
| Nausea | 33% | 51% | 9% | 76% | 77% |
| Diarrhea | 25% | 45% | 29% | 45% | 26% |
| Vomiting | 23% | 37% | 28% | 53% | 49% |
| Nausea and vomiting | 8% | 14% | 11% | 18% | 9% |
| Anorexia | 14% | 24% | 16% | 31% | 26% |
| Heme & Lymphatic | |||||
| Anemia | 4% | 14% | 9% | 36% | 26% |
| Leukopenia | 3% | 24% | 17% | 52% | 34% |
| Metabolic | |||||
| Peripheral edema | 10% | 22% | 20% | 20% | 17% |
| Edema | 8% | 10% | 8% | 11% | 5% |
| Musculoskeletal | |||||
| Bone pain | 7% | 24% | 18% | 7% | 7% |
| Arthralgia | 6% | 37% | 21% | 8% | 9% |
| Nervous | |||||
| Insomnia | 14% | 25% | 13% | 29% | 15% |
| Dizziness | 13% | 22% | 24% | 24% | 18% |
| Paresthesia | 9% | 48% | 39% | 17% | 11% |
| Depression | 6% | 12% | 13% | 20% | 12% |
| Peripheral neuritis | 2% | 23% | 16% | 2% | 2% |
| Neuropathy | 1% | 13% | 5% | 4% | 4% |
| Respiratory | |||||
| Cough increased | 26% | 41% | 22% | 43% | 29% |
| Dyspnea | 22% | 27% | 26% | 42% | 25% |
| Rhinitis | 14% | 22% | 5% | 22% | 16% |
| Pharyngitis | 12% | 22% | 14% | 30% | 18% |
| Sinusitis | 9% | 21% | 7% | 13% | 6% |
| Skin | |||||
| Rash | 18% | 38% | 18% | 27% | 17% |
| Herpes simplex | 2% | 12% | 3% | 7% | 9% |
| Acne | 2% | 11% | 3% | 3% | <1% |
| Urogenital | |||||
| Urinary tract infection | 5% | 18% | 14% | 13% | 7% |
a Data for trastuzumab single agent were from 4 studies, including 213 patients from Study 6.
b Anthracycline (doxorubicin or epirubicin) and cyclophosphamide.
Metastatic Gastric Cancer
The data below are based on the exposure of 294 patients to trastuzumab in combination with a fluoropyrimidine (capecitabine or 5-FU) and cisplatin (Study 7). In the trastuzumab plus chemotherapy arm, the initial dose of trastuzumab 8 mg/kg was administered on Day 1 (prior to chemotherapy) followed by 6 mg/kg every 21 days until disease progression. Cisplatin was administered at 80 mg/m² on Day 1 and the fluoropyrimidine was administered as either capecitabine 1000 mg/m² orally twice a day on Days 1–14 or 5- fluorouracil 800 mg/m² /day as a continuous intravenous infusion Days 1 through 5. Chemotherapy was administered for six 21-daycycles. Median duration of trastuzumab treatment was 21 weeks; median number of trastuzumab infusions administered was eight.
Table 5. Study 7: Per Patient Incidence of Adverse Reactions of All Grades (Incidence ≥ 5% between Arms) or Grade ¾ (Incidence > 1% between Arms) and Higher Incidence in Trastuzumab Arm:
| Body System/Adverse Event | Trastuzumab + FC (N = 294) N (%) | FC (N = 290) N (%) | ||
|---|---|---|---|---|
| All Grades | Grades 3/4 | All Grades | Grades 3/4 | |
| Investigations | ||||
| Neutropenia | 230 (78) | 101 (34) | 212 (73) | 83 (29) |
| Hypokalemia | 83 (28) | 28 (10) | 69 (24) | 16 (6) |
| Anemia | 81 (28) | 36 (12) | 61 (21) | 30 (10) |
| Thrombocytopenia | 47 (16) | 14 (5) | 33 (11) | 8 (3) |
| Blood and Lymphatic System Disorders | ||||
| Febrile Neutropenia | - | 15 (5) | - | 8 (3) |
| Gastrointestinal Disorders | ||||
| Diarrhea | 109 (37) | 27 (9) | 80 (28) | 11 (4) |
| Stomatitis | 72 (24) | 2 (1) | 43 (15) | 6 (2) |
| Dysphagia | 19 (6) | 7 (2) | 10 (3) | 1 (≤ 1) |
| Body as a Whole | ||||
| Fatigue | 102 (35) | 12 (4) | 82 (28) | 7 (2) |
| Fever | 54 (18) | 3 (1) | 36 (12) | 0 (0) |
| Mucosal Inflammation | 37 (13) | 6 (2) | 18 (6) | 2 (1) |
| Chills | 23 (8) | 1 (≤ 1) | 0 (0) | 0 (0) |
| Metabolism and Nutrition Disorders | ||||
| Weight Decrease | 69 (23) | 6 (2) | 40 (14) | 7 (2) |
| Infections and Infestations | ||||
| Upper Respiratory Tract Infections | 56 (19) | 0 (0) | 29 (10) | 0 (0) |
| Nasopharyngitis | 37 (13) | 0 (0) | 17 (6) | 0 (0) |
| Renal and Urinary Disorders | ||||
| Renal Failure and Impairment | 53 (18) | 8 (3) | 42 (15) | 5 (2) |
| Nervous System Disorders | ||||
| Dysgeusia | 28 (10) | 0 (0) | 14 (5) | 0 (0) |
The following subsections provide additional detail regarding adverse reactions observed in clinical trials of adjuvant breast cancer, metastatic breast cancer, metastatic gastric cancer, or post-marketing experience.
Cardiomyopathy
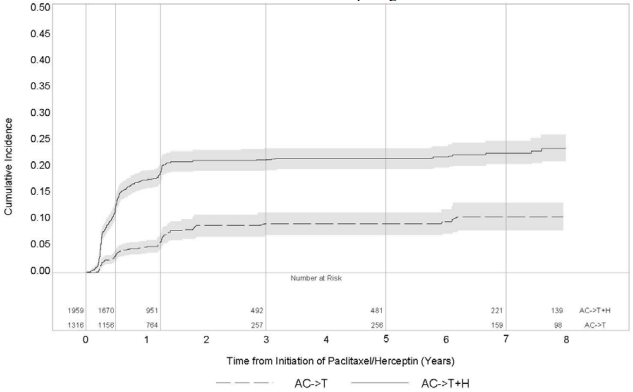
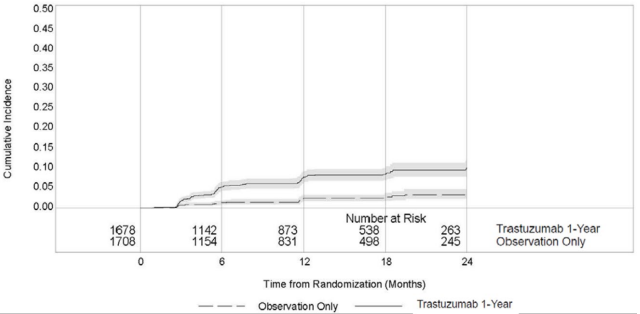
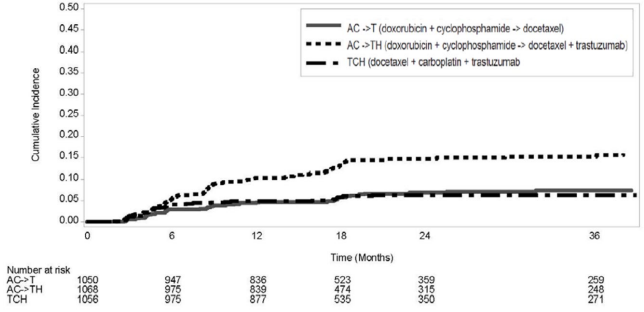
Serial measurement of cardiac function (LVEF) was obtained in clinical trials in the adjuvant treatment of breast cancer. In Study 3, the median duration of follow-up was 12.6 months (12.4 months in the observation arm; 12.6 months in the 1-year trastuzumab arm); and in Studies 1 and 2, 7.9 years in the AC-T arm, 8.3 years in the AC-TH arm. In Studies 1 and 2, 6% of all randomized patients with post-AC LVEF evaluation were not permitted to initiate trastuzumab following completion of AC chemotherapy due to cardiac dysfunction (LVEF < LLN or ≥ 16 point decline in LVEF from baseline to end of AC). Following initiation of trastuzumab therapy, the incidence of new-onset dose-limiting myocardial dysfunction was higher among patients receiving trastuzumab and paclitaxel as compared to those receiving paclitaxel alone in Studies 1 and 2, and in patients receiving one-year trastuzumab monotherapy compared to observation in Study 3 (see Table 6, Figures 1 and 2). The per-patient incidence of new-onset cardiac dysfunction, as measured by LVEF, remained similar when compared to the analysis performed at a median follow-up of 2.0 years in the AC-TH arm. This analysis also showed evidence of reversibility of left ventricular dysfunction, with 64.5% of patients who experienced symptomatic CHF in the AC-TH group being asymptomatic at latest follow-up, and 90.3% having full or partial LVEF recovery.
Table 6a. Per-patient Incidence of New Onset Myocardial Dysfunction (by LVEF) Studies 1, 2, 3 and 4:
| LVEF < 50% and Absolute Decrease from Baseline | Absolute LVEF Decrease | ||||
|---|---|---|---|---|---|
| LVEF < 50% | ≥ 10% decrease | ≥ 16% decrease | < 20% and ≥ 10% | ≥ 20% | |
| Studies 1 & 2b,c | |||||
| AC→TH (n = 1856) | 23.1% (428) | 18.5% (344) | 11.2% (208) | 37.9% (703) | 8.9% (166) |
| AC→T (n = 1170) | 11.7% (137) | 7.0% (82) | 3.0% (35) | 22.1% (259) | 3.4% (40) |
| Study 3d | |||||
| Trastuzumab (n = 1678) | 8.6% (144) | 7.0% (118) | 3.8% (64) | 22.4% (376) | 3.5% (59) |
| Observation (n = 1708) | 2.7% (46) | 2.0% (35) | 1.2% (20) | 11.9% (204) | 1.2% (21) |
| Study 4e | |||||
| TCH (n = 1056) | 8.5% (90) | 5.9% (62) | 3.3% (35) | 34.5% (364) | 6.3% (67) |
| AC→TH (n = 1068) | 17% (182) | 13.3% (142) | 9.8% (105) | 44.3% (473) | 13.2% (141) |
| AC→T (n = 1050) | 9.5% (100) | 6.6% (69) | 3.3% (35) | 34% (357) | 5.5% (58) |
a For Studies 1, 2 and 3, events are counted from the beginning of trastuzumab treatment. For Study 4, events are counted from the date of randomization.
b Studies 1 and 2 regimens: doxorubicin and cyclophosphamide followed by paclitaxel (AC→T) or paclitaxel plus trastuzumab (AC→TH).
c Median duration of follow-up for Studies 1 and 2 combined was 8.3 years in the AC→TH arm.
d Median follow-up duration of 12.6 months in the one-year trastuzumab treatment arm.
e Study 4 regimens: doxorubicin and cyclophosphamide followed by docetaxel (AC→T) or docetaxel plus trastuzumab (AC→TH); docetaxel and carboplatin plus trastuzumab (TCH).
Figure 1. Studies 1 and 2: Cumulative Incidence of Time to First LVEF Decline of ≥ 10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event:
Time 0 is initiation of paclitaxel or trastuzumab + paclitaxel therapy.
Figure 2. Study 3: Cumulative Incidence of Time to First LVEF Decline of ≥ 10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event:
Figure 3. Study 4: Cumulative Incidence of Time to First LVEF Decline of ≥ 10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event:
Time 0 is the date of randomization.
The incidence of treatment emergent congestive heart failure among patients in the metastatic breast cancer trials was classified for severity using the New York Heart Association classification system (I−IV, where IV is the most severe level of cardiac failure) (see Table 2). In the metastatic breast cancer trials, the probability of cardiac dysfunction was highest in patients who received trastuzumab concurrently with anthracyclines.
In Study 7, 5.0% of patients in the trastuzumab plus chemotherapy arm compared to 1.1% of patients in the chemotherapy alone arm had LVEF value below 50% with a ≥ 10% absolute decrease in LVEF from pretreatment values.
Infusion Reactions
During the first infusion with trastuzumab, the symptoms most commonly reported were chills and fever, occurring in approximately 40% of patients in clinical trials. Symptoms were treated with acetaminophen, diphenhydramine, and meperidine (with or without reduction in the rate of trastuzumab infusion); permanent discontinuation of trastuzumab for infusion reactions was required in < 1% of patients. Other signs and/or symptoms may include nausea, vomiting, pain (in some cases at tumor sites), rigors, headache, dizziness, dyspnea, hypotension, elevated blood pressure, rash, and asthenia. Infusion reactions occurred in 21% and 35% of patients, and were severe in 1.4% and 9% of patients, on second or subsequent trastuzumab infusions administered as monotherapy or in combination with chemotherapy, respectively. In the post-marketing setting, severe infusion reactions, including hypersensitivity, anaphylaxis, and angioedema have been reported.
Anemia
In randomized controlled clinical trials, the overall incidence of anemia (30% vs. 21% [Study 5]), of selected NCI-CTC Grade 2–5 anemia (12.3% vs. 6.7% [Study 1]), and of anemia requiring transfusions (0.1% vs. 0 patients [Study 2]) were increased in patients receiving trastuzumab and chemotherapy compared with those receiving chemotherapy alone. Following the administration of trastuzumab as a single agent (Study 6), the incidence of NCI-CTC Grade 3 anemia was < 1%. In Study 7 (metastatic gastric cancer), on the trastuzumab containing arm as compared to the chemotherapy alone arm, the overall incidence of anemia was 28% compared to 21% and of NCI CTC Grade ¾ anemia was 12.2% compared to 10.3%.
Neutropenia
In randomized controlled clinical trials in the adjuvant setting, the incidence of selected NCI-CTC Grade 4−5 neutropenia (1.7% vs. 0.8% [Study 2]) and of selected Grade 2−5 neutropenia (6.4% vs. 4.3% [Study 1]) were increased in patients receiving trastuzumab and chemotherapy compared with those receiving chemotherapy alone. In a randomized, controlled trial in patients with metastatic breast cancer, the incidences of NCI-CTC Grade ¾ neutropenia (32% vs. 22%) and of febrile neutropenia (23% vs. 17%) were also increased in patients randomized to trastuzumab in combination with myelosuppressive chemotherapy as compared to chemotherapy alone. In Study 7 (metastatic gastric cancer) on the trastuzumab containing arm as compared to the chemotherapy alone arm, the incidence of NCI-CTC Grade ¾ neutropenia was 36.8% compared to 28.9%; febrile neutropenia 5.1% compared to 2.8%.
Infection
The overall incidences of infection (46% vs. 30% [Study 5]), of selected NCI-CTC Grade 2−5 infection/febrile neutropenia (24.3% vs. 13.4% [Study 1]) and of selected Grade 3−5 infection/febrile neutropenia (2.9% vs. 1.4% [Study 2]) were higher in patients receiving trastuzumab and chemotherapy compared with those receiving chemotherapy alone. The most common site of infections in the adjuvant setting involved the upper respiratory tract, skin, and urinary tract.
In Study 4, the overall incidence of infection was higher with the addition of trastuzumab to AC-T but not to TCH [44% (AC-TH), 37% (TCH), 38% (AC-T)]. The incidences of NCI-CTC Grade 3-4 infection were similar [25% (AC-TH), 21% (TCH), 23% (AC-T)] across the three arms.
In a randomized, controlled trial in treatment of metastatic breast cancer, the reported incidence of febrile neutropenia was higher (23% vs. 17%) in patients receiving trastuzumab in combination with myelosuppressive chemotherapy as compared to chemotherapy alone.
Pulmonary Toxicity
Adjuvant Breast Cancer:
Among women receiving adjuvant therapy for breast cancer, the incidence of selected NCI-CTC Grade 2-5 pulmonary toxicity (14.3% vs. 5.4% [Study 1]) and of selected NCI-CTC Grade 3-5 pulmonary toxicity and spontaneous reported Grade 2 dyspnea (3.4% vs. 0.9% [Study 2]) was higher in patients receiving trastuzumab and chemotherapy compared with chemotherapy alone. The most common pulmonary toxicity was dyspnea (NCI-CTC Grade 2-5: 11.8% vs. 4.6% [Study 1]; NCI-CTC Grade 2-5: 2.4% vs. 0.2% [Study 2]).
Pneumonitis/pulmonary infiltrates occurred in 0.7% of patients receiving trastuzumab compared with 0.3% of those receiving chemotherapy alone. Fatal respiratory failure occurred in 3 patients receiving trastuzumab, one as a component of multi-organ system failure, as compared to 1 patient receiving chemotherapy alone.
In Study 3, there were 4 cases of interstitial pneumonitis in the one-year trastuzumab treatment arm compared to none in the observation arm at a median follow-up duration of 12.6 months.
Metastatic Breast Cancer:
Among women receiving trastuzumab for treatment of metastatic breast cancer, the incidence of pulmonary toxicity was also increased. Pulmonary adverse events have been reported in the post- marketing experience as part of the symptom complex of infusion reactions. Pulmonary events include bronchospasm, hypoxia, dyspnea, pulmonary infiltrates, pleural effusions, non-cardiogenic pulmonary edema, and acute respiratory distress syndrome. For a detailed description, see Warnings and Precautions (5.4).
Thrombosis / Embolism
In 4 randomized, controlled clinical trials, the incidence of thrombotic adverse events was higher in patients receiving trastuzumab and chemotherapy compared to chemotherapy alone in three studies (2.6% vs. 1.5% [Study 1], 2.5% and 3.7% vs. 2.2% [Study 4] and 2.1% vs. 0% [Study 5]).
Diarrhea
Among women receiving adjuvant therapy for breast cancer, the incidence of NCI-CTC Grade 2-5 diarrhea (6.7% vs. 5.4% [Study 1]) and of NCI-CTC Grade 3-5 diarrhea (2.2% vs. 0% [Study 2]), and of Grade 1-4 diarrhea (7% vs. 1% [Study 3; one-year trastuzumab treatment at 12.6 months median duration of followup]) were higher in patients receiving trastuzumab as compared to controls. In Study 4, the incidence of Grade 3-4 diarrhea was higher [5.7% AC-TH, 5.5% TCH vs. 3.0% AC-T] and of Grade 1-4 was higher [51% AC-TH, 63% TCH vs. 43% AC-T] among women receiving trastuzumab. Of patients receiving trastuzumab as a single agent for the treatment of metastatic breast cancer, 25% experienced diarrhea. An increased incidence of diarrhea was observed in patients receiving trastuzumab in combination with chemotherapy for treatment of metastatic breast cancer.
Renal Toxicity
In Study 7 (metastatic gastric cancer) on the trastuzumab-containing arm as compared to the chemotherapy alone arm the incidence of renal impairment was 18% compared to 14.5%. Severe (Grade ¾) renal failure was 2.7% on the trastuzumab-containing arm compared to 1.7% on the chemotherapy only arm. Treatment discontinuation for renal insufficiency/failure was 2% on the trastuzumab-containing arm and 0.3% on the chemotherapy only arm.
In the post-marketing setting, rare cases of nephrotic syndrome with pathologic evidence of glomerulopathy have been reported. The time to onset ranged from 4 months to approximately 18 months from initiation of trastuzumab therapy. Pathologic findings included membranous glomerulonephritis, focal glomerulosclerosis, and fibrillary glomerulonephritis. Complications included volume overload and congestive heart failure.
6.2. Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and the specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other trastuzumab products may be misleading.
Among 903 women with metastatic breast cancer, human anti-human antibody (HAHA) to trastuzumab was detected in one patient using an enzyme-linked immunosorbent assay (ELISA). This patient did not experience an allergic reaction. Samples for assessment of HAHA were not collected in studies of adjuvant breast cancer.
6.3. Postmarketing Experience
The following adverse reactions have been identified during post-approval use of trastuzumab. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Infusion reaction [see Warnings and Precautions (5.2)]
- Oligohydramnios or oligohydramnios sequence, including pulmonary hypoplasia, skeletal abnormalities, and neonatal death [see Warnings and Precautions (5.3)]
- Glomerulopathy [see Adverse Reactions (6.1)]
- Immune thrombocytopenia
- Tumor lysis syndrome (TLS): Cases of possible TLS have been reported in patients treated with trastuzumab. Patients with significant tumor burden (e.g. bulky metastases) may be at a higher risk. Patients could present with hyperuricemia, hyperphosphatemia, and acute renal failure which may represent possible TLS. Providers should consider additional monitoring and/or treatment as clinically indicated.
7. Drug Interactions
Patients who receive anthracycline after stopping trastuzumab products may be at increased risk of cardiac dysfunction because of trastuzumab’s long washout period based on population PK analysis [see Clinical Pharmacology (12.3)]. If possible, physicians should avoid anthracycline-based therapy for up to 7 months after stopping trastuzumab products. If anthracyclines are used, the patient’s cardiac function should be monitored carefully.
8.1. Pregnancy
Risk Summary
Trastuzumab products can cause fetal harm when administered to a pregnant woman. In post-marketing reports, use of trastuzumab during pregnancy resulted in cases of oligohydramnios and of oligohydramnios sequence, manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death [see Data]. Apprise the patient of the potential risks to a fetus. There are clinical considerations if a trastuzumab product is used in a pregnant woman or if a patient becomes pregnant within 7 months following the last dose of a trastuzumab product [see Clinical Considerations].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Fetal / Neonatal Adverse Reactions
Monitor women who received Hercessi during pregnancy or within 7 months prior to conception for oligohydramnios. If oligohydramnios occurs, perform fetal testing that is appropriate for gestational age and consistent with community standards of care.
Data
Human Data
In post-marketing reports, use of trastuzumab during pregnancy resulted in cases of oligohydramnios and of oligohydramnios sequence, manifesting in the fetus as pulmonary hypoplasia, skeletal abnormalities, and neonatal death. These case reports described oligohydramnios in pregnant women who received trastuzumab either alone or in combination with chemotherapy. In some case reports, amniotic fluid index increased after trastuzumab was stopped. In one case, trastuzumab therapy resumed after amniotic index improved and oligohydramnios recurred.
Animal Data
In studies where trastuzumab was administered to pregnant cynomolgus monkeys during the period of organogenesis at doses up to 25 mg/kg given twice weekly (up to 25 times the recommended weekly human dose of 2 mg/kg), trastuzumab crossed the placental barrier during the early (Gestation Days 20 to 50) and late (Gestation Days 120 to 150) phases of gestation. The resulting concentrations of trastuzumab in fetal serum and amniotic fluid were approximately 33% and 25%, respectively, of those present in the maternal serum but were not associated with adverse developmental effects.
8.2. Lactation
Risk Summary
There is no information regarding the presence of trastuzumab products in human milk, the effects on thebreastfed infant, or the effects on milk production. Published data suggest human IgG is present in human milk but does not enter the neonatal and infant circulation in substantial amounts. Trastuzumab was present in the milk of lactating cynomolgus monkeys but not associated with neonatal toxicity [see Data]. Consider the developmental and health benefits of breastfeeding along with the mother’s clinical need for Hercessi treatment and any potential adverse effects on the breastfed child from Hercessi or from the underlying maternal condition. This consideration should also take into account the trastuzumab product wash out period of 7 months [see Clinical Pharmacology (12.3)].
Data
In lactating cynomolgus monkeys, trastuzumab was present in breast milk at about 0.3% of maternal serum concentrations after pre- (beginning Gestation Day 120) and post-partum (through Post-partum Day 28) doses of 25 mg/kg administered twice weekly (25 times the recommended weekly human dose of 2 mg/kg of trastuzumab products). Infant monkeys with detectable serum levels of trastuzumab did not exhibit any adverse effects on growth or development from birth to 1 month of age.
8.3. Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to the initiation of Hercessi.
Contraception
Females
Trastuzumab products can cause embryo-fetal harm when administered during pregnancy. Advise females of reproductive potential to use effective contraception during treatment with Hercessi and for 7 months following the last dose of Hercessi [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.3)].
8.4. Pediatric Use
The safety and effectiveness of Hercessi in pediatric patients have not been established.
8.5. Geriatric Use
Trastuzumab has been administered to 386 patients who were 65 years of age or over (253 in the adjuvant treatment and 133 in metastatic breast cancer treatment settings). The risk of cardiac dysfunction was increased in geriatric patients as compared to younger patients in both those receiving treatment for metastatic disease in Studies 5 and 6, or adjuvant therapy in Studies 1 and 2. Limitations in data collection and differences in study design of the 4 studies of trastuzumab in adjuvant treatment of breast cancer preclude a determination of whether the toxicity profile of trastuzumab in older patients is different from younger patients. The reported clinical experience is not adequate to determine whether the efficacy improvements (ORR, TTP, OS, DFS) of trastuzumab treatment in older patients is different from that observed in patients < 65 years of age for metastatic disease and adjuvant treatment.
In Study 7 (metastatic gastric cancer), of the 294 patients treated with trastuzumab, 108 (37%) were 65 years of age or older, while 13 (4.4%) were 75 and over. No overall differences in safety or effectiveness were observed.
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.