XEOMIN Powder for solution for injection Ref.[11109] Active ingredients: Botulinum toxin type A
Source: FDA, National Drug Code (US) Revision Year: 2021
1. Indications and Usage
1.1 Chronic Sialorrhea
XEOMIN is indicated for the treatment of chronic sialorrhea in patients 2 years of age and older.
1.2 Upper Limb Spasticity
Upper Limb Spasticity in Adult Patients
XEOMIN is indicated for the treatment of upper limb spasticity in adult patients.
Upper Limb Spasticity in Pediatric Patients, Excluding Spasticity Caused by Cerebral Palsy
XEOMIN is indicated for the treatment of upper limb spasticity in pediatric patients 2 to 17 years of age, excluding spasticity caused by cerebral palsy.
1.3 Cervical Dystonia
XEOMIN is indicated for the treatment of cervical dystonia in adult patients.
1.4 Blepharospasm
XEOMIN is indicated for the treatment of blepharospasm in adult patients.
1.5 Glabellar Lines
XEOMIN is indicated for the temporary improvement in the appearance of moderate to severe glabellar lines associated with corrugator and/or procerus muscle activity in adult patients.
2. Dosage and Administration
2.1 Instructions for Safe Use
The potency Units of XEOMIN for injection are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products and, therefore, units of biological activity of XEOMIN cannot be compared to or converted into Units of any other botulinum toxin products assessed with any other specific assay method [see Warnings and Precautions (5.2) and Description (11)]. Reconstituted XEOMIN is intended for intramuscular or intra-salivary gland injection only.
The recommended maximum cumulative dose for any indication should not exceed 400 Units in a treatment session.
2.2 Chronic Sialorrhea
Chronic Sialorrhea in Adult Patients
XEOMIN is injected into the parotid and submandibular glands on both sides (i.e., 4 injection sites per treatment session). The recommended total dose per treatment session is 100 Units. The dose is divided with a ratio of 3:2 between the parotid and submandibular glands (Table 1).
Figure 1. Glands for Injection in Chronic Sialorrhea in Adult Patients:
Use the following guidelines if locating salivary glands using anatomic landmarks:
- To inject the parotid gland, find the midpoint on the line connecting the tragus and mandible angle (Site A and B, respectively, Figure 1), approximately at the height of the ear lobe. Deliver the injection one finger breadth anterior to this site (Star 1, Figure 1).
- To inject the submandibular gland, find the midpoint between the angle of the mandible and the tip of the chin (Site B and C, respectively, Figure 1). Deliver the injection one finger breadth medial to the inferior surface of the mandible at this site (Star 2, Figure 1).
Table 1. Dosing by Gland for Treatment of Chronic Sialorrhea in Adult Patients:
| Gland(s) | Units Per Side | Total |
|---|---|---|
| Parotid gland(s) | 30 Units | 60 Units |
| Submandibular gland(s) | 20 Units | 40 Units |
| Both Glands | 50 Units | 100 Units |
The concentration used in the clinical study after reconstitution was 5 Units/0.1mL. The timing for repeat treatment should be determined based on the actual clinical need of the individual patient, and no sooner than every 16 weeks.
Chronic Sialorrhea in Pediatric Patients
XEOMIN is injected into the parotid and submandibular glands on both sides (i.e., 4 injection sites per treatment session). Ultrasound imaging is recommended to guide needle placement into the salivary glands. The body-weight adjusted dose is divided with a ratio of 3:2 between the parotid and submandibular glands (Table 2). XEOMIN has not been studied in children weighing less than 12 kg [see Clinical Studies (14.1)].
Figure 2. Glands for Injection in Chronic Sialorrhea in Pediatric Patients:
Table 2. Dosing by Body Weight Class for Treatment of Chronic Sialorrhea in Pediatric Patients:
| Body weight | Parotid gland, each side | Submandibular gland, each side | Total dose, both glands, both sides | ||
|---|---|---|---|---|---|
| Dose per gland | Volume per injection | Dose per gland | Volume per injection | ||
| 12 kg or more to less than 15 kg | 6 Units | 0.24 mL | 4 Units | 0.16 mL | 20 Units |
| 15 kg or more to less than 19 kg | 9 Units | 0.36 mL | 6 Units | 0.24 mL | 30 Units |
| 19 kg or more to less than 23 kg | 12 Units | 0.48 mL | 8 Units | 0.32 mL | 40 Units |
| 23 kg or more to less than 27 kg | 15 Units | 0.6 mL | 10 Unts | 0.4 mL | 50 Units |
| 27 kg or more to less than 30 kg | 18 Units | 0.72 mL | 12 Units | 0.48 mL | 60 Units |
| 30 kg or more | 22.5 Units | 0.9 mL | 15 Units | 0.6 mL | 75 Units |
The concentration used in the clinical study after reconstitution was 2.5 Units/0.1 mL. The timing for repeat treatment should be determined based on the actual clinical need of the individual patient, and no sooner than every 16 weeks.
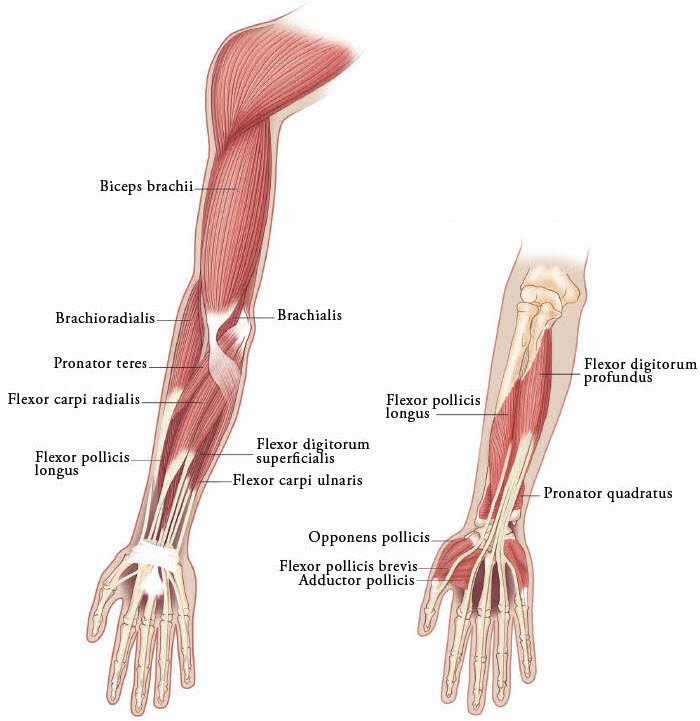
2.3 Upper Limb Spasticity
Upper Limb Spasticity in Adult Patients
The dosage, frequency, and number of injection sites should be tailored to the individual patient based on the size, number, and location of muscles to be treated, severity of spasticity, presence of local muscle weakness, patient’s response to previous treatment, and adverse event history with XEOMIN. The frequency of XEOMIN treatments should be no sooner than every 12 weeks. In patients not previously treated with a botulinum toxin, initial dosing should begin at the low end of the recommended dosing range and titrated as clinically necessary. Most patients in clinical studies were retreated between 12 and 14 weeks.
Table 3. XEOMIN Dosing by Muscle for Treatment of Adult Upper Limb Spasticity:
| Clinical Pattern Muscle | Units (Range) | Number of injection sites per muscle |
|---|---|---|
| Clenched Fist | ||
| Flexor digitorum superficialis | 25 Units-100 Units | 2 |
| Flexor digitorum profundus | 25 Units-100 Units | 2 |
| Flexed Wrist | ||
| Flexor carpi radialis | 25 Units-100 Units | 1-2 |
| Flexor carpi ulnaris | 20 Units-100 Units | 1-2 |
| Flexed Elbow | ||
| Brachioradialis | 25 Units-100 Units | 1-3 |
| Biceps | 50 Units-200 Units | 1-4 |
| Brachialis | 25 Units-100 Units | 1-2 |
| Pronated Forearm | ||
| Pronator quadratus | 10 Units-50 Units | 1 |
| Pronator teres | 25 Units-75 Units | 1-2 |
| Thumb-in-Palm | ||
| Flexor pollicis longus | 10 Units-50 Units | 1 |
| Adductor pollicis | 5 Units-30 Units | 1 |
| Flexor pollicis brevis/Opponens pollicis | 5 Units-30 Units | 1 |
Figure 3. Muscles Involved In Adult Upper Limb Spasticity:
Upper Limb Spasticity in Pediatric Patients, Excluding Spasticity Caused by Cerebral Palsy
The exact dosage, frequency, and number of injection sites should be tailored to the individual patient based on size, number and localization of involved muscles; the severity of spasticity; and the presence of local muscle weakness.
The maximum recommended dose is 8 Units/kg, divided among affected muscles, up to a maximum dose of 200 Units per single upper limb. If both upper limbs are treated, total XEOMIN dosage should not exceed 16 Units/kg, up to a maximum of 400 Units.
Based on the selected dose, a reconstituted solution at a concentration between 1.25 Units/0.1 mL and 5 Units/0.1 mL is recommended [see Dosage and Administration (2.7)]. The timing for repeat treatment should be determined based on the clinical need of the patient; the frequency of repeat treatments should be no sooner than every 12 weeks. Most patients in clinical studies were retreated between 12 and 16 weeks.
Table 4 includes the recommended dose ranges for the treatment of the clinical patterns of flexed elbow, flexed wrist, pronated forearm, clenched fist, and thumb-in-palm.
Table 4. XEOMIN Dosing by Muscle for Treatment of Pediatric Upper Limb Spasticity, Excluding Spasticity Caused by Cerebral Palsy:
| Clinical Pattern Muscle | Dosage | Number of Injection Sites per Muscle | |
|---|---|---|---|
| Range (Units/kg) | Maximum (Units) | ||
| Flexed Elbow | |||
| Brachioradialis | 1-2 | 50 | 1-2 |
| Biceps | 2-3 | 75 | 1-3 |
| Brachialis | 1-2 | 50 | 1-2 |
| Flexed Wrist | |||
| Flexor carpi radialis | 1 | 25 | 1 |
| Flexor carpi ulnaris | 1 | 25 | 1 |
| Pronated Forearm | |||
| Pronator quadratus | 0.5 | 12.5 | 1 |
| Pronator teres | 1-2 | 50 | 1-2 |
| Clenched Fist | |||
| Flexor digitorum superficialis | 1 | 25 | 1 |
| Flexor digitorum profundus | 1 | 25 | 1 |
| Thumb-in-Palm | |||
| Flexor pollicis longus | 1 | 25 | 1 |
| Adductor pollicis | 0.5 | 12.5 | 1 |
| Flexor pollicis brevis/ opponens pollicis | 0.5 | 12.5 | 1 |
Figure 4. Muscles Injected for Pediatric Upper Limb Spasticity:
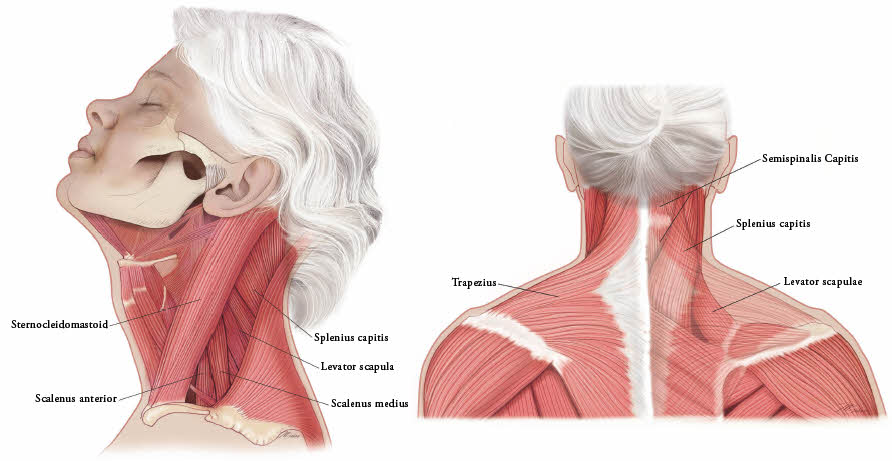
2.4 Cervical Dystonia
The recommended initial dose of XEOMIN for cervical dystonia is 120 Units. In a placebo-controlled trial utilizing initial XEOMIN doses of 120 Units and 240 Units, no meaningful difference in effectiveness was demonstrated between the doses [see Clinical Studies (14.3)]. In previously treated patients, their past dose, response to treatment, duration of effect, and adverse event history should be taken into consideration when determining the XEOMIN dose.
In the treatment of cervical dystonia, XEOMIN is usually injected into the sternocleidomastoid, levator scapulae, splenius capitis, scalenus, and/or the trapezius muscle(s) (see Figure 5). This list is not exhaustive, as any of the muscles responsible for controlling head position may require treatment [see Clinical Studies (14.3)]. The dose and number of injection sites in each treated muscle should be individualized based on the number and location of the muscle(s) to be treated, the degree of spasticity/dystonia, muscle mass, body weight, and response to any previous botulinum toxin injections.
The frequency of XEOMIN repeat treatments should be determined by clinical response, but should generally be no more frequent than every 12 weeks [see Clinical Studies (14.3)].
Figure 5. Muscles Involved in Cervical Dsytonia:
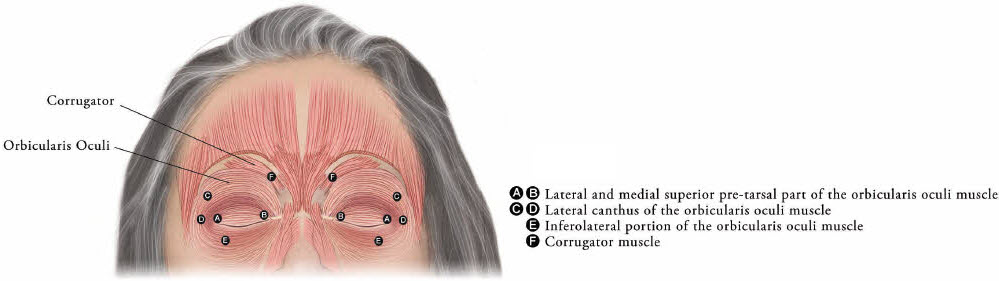
2.5 Blepharospasm
In treatment-naïve patients, the recommended initial dose of XEOMIN is 50 Units (25 Units per eye). In patients previously treated with a botulinum toxin A, their past dose, response to treatment, duration of effect, and adverse event history should be taken into consideration when determining the XEOMIN dose.
The total dose of XEOMIN should not exceed 100 Units per treatment session (50 Units per eye).
XEOMIN is injected into the lateral and medial orbicularis oculi muscle of the upper lid; lateral canthus and the lateral orbicularis oculi muscle of the lower lid; and the corrugator muscle, if necessary (see Figure 6). The number and location of injections may be changed in response to adverse reactions or based on the patient’s response to treatment, but the total dose should not exceed 50 Units per eye.
Figure 6. Injection Sites for Blepharospasm:
The frequency of XEOMIN repeat treatments should be determined by clinical response but should generally be no more frequent than every 12 weeks [see Clinical Studies (14.4)].
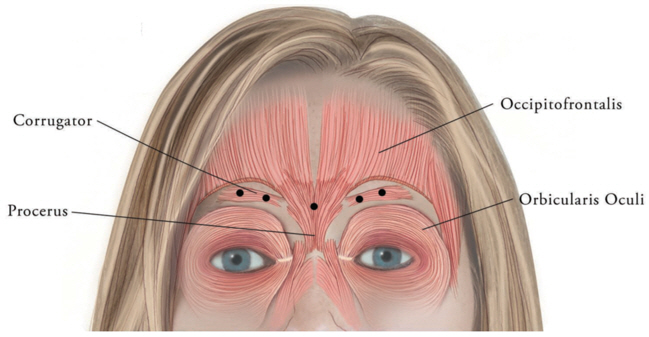
2.6 Glabellar Lines
The total recommended XEOMIN dose is 20 Units per treatment session divided into five equal intramuscular injections of 4 Units each. The five injection sites are: two injections in each corrugator muscle and one injection in the procerus muscle.
Retreatment with XEOMIN should be administered no more frequently than every three months.
Figure 7. Injection Sites for Glabellar Lines:
2.7 Preparation and Reconstitution Technique
Prior to injection, reconstitute each vial of XEOMIN with sterile, preservative-free 0.9% Sodium Chloride Injection, USP [see Dosage Form and Strengths (3)]. A 20-27 gauge short bevel needle is recommended for reconstitution. Draw up an appropriate amount of preservative-free 0.9% Sodium Chloride Injection, USP into a syringe (see Table 5). Clean the exposed portion of the rubber stopper of the vial with alcohol (70%) prior to insertion of the needle. After vertical insertion of the needle through the rubber stopper, the vacuum will draw the saline into the vial. Gently inject any remaining saline into the vial to avoid foam formation. If the vacuum does not pull the saline into the vial, then XEOMIN must be discarded. Remove the syringe from the vial and mix XEOMIN with the saline by carefully swirling and inverting/flipping the vial – do not shake vigorously. Reconstituted XEOMIN is a clear, colorless solution free of particulate matter. XEOMIN should not be used if the reconstituted solution has a cloudy appearance or contains floccular or particulate matter.
After reconstitution, XEOMIN should be used for only one injection session and for only one patient. Reconstituted XEOMIN solution should be administered within 24 hours after dilution. During this time period, unused reconstituted XEOMIN may be stored in the original container in a refrigerator 2°C-8°C (36°F-46°F) for up to 24 hours until time of use. XEOMIN vials are for single-dose only. Discard any unused portion.
Diluent volumes for reconstitution of XEOMIN are indicated in Table 5.
Table 5. Diluent Volumes for Reconstitution of XEOMIN:
| Volume of preservative-free 0.9% Sodium Chloride Injection, USP | 50 Unit Vial: Resulting dose in Units per 0.1 mL | 100 Unit Vial: Resulting dose in Units per 0.1 mL | 200 Unit Vial: Resulting dose in Units per 0.1 mL |
|---|---|---|---|
| 0.25 mL | 20 Units | - | - |
| 0.5 mL | 10 Units | 20 Units | 40 Units |
| 1 mL | 5 Units | 10 Units | 20 Units |
| 1.25 mL | 4 Units | 8 Units | 16 Units |
| 2 mL | 2.5 Units | 5 Units | 10 Units |
| 2.5 mL | 2 Units | 4 Units | 8 Units |
| 4 mL | 1.25 Units | 2.5 Units | 5 Units |
| 5 mL | 1 Unit | 2 Units | 4 Units |
| 8 mL* | - | 1.25 Units | 2.5 Units |
| 16 mL† | - | - | 1.25 Units |
* When using 8 mL of diluent for a 100 Unit or 200 Unit vial of XEOMIN, complete the following steps:
1. Reconstitute a 100 Unit or 200 Unit vial of XEOMIN with 4 mL of preservative-free 0.9% Sodium Chloride Injection, USP, following instructions above.
2. Withdraw 4 mL of preservative-free 0.9% Sodium Chloride Injection, USP, into an appropriately sized syringe for 8 mL in total.
3. Using the same syringe, draw up the 4 mL of XEOMIN solution from the reconstituted vial and mix gently.
†When using 16 mL of diluent for a 200 Unit vial of XEOMIN, complete the following steps:
1. Reconstitute a 200 Unit vial of XEOMIN with 4 mL of preservative-free 0.9% Sodium Chloride Injection, USP, following instructions above.
2. Withdraw 12 mL of preservative-free 0.9% Sodium Chloride Injection, USP, into an appropriately sized syringe for 16 mL in total.
3. Using the same syringe, draw up the 4 mL of XEOMIN solution from the reconstituted vial and mix gently.
2.8 Administration
Reconstituted XEOMIN is intended for intramuscular or intra-salivary gland injection only.
If proposed injection sites are marked with a pen, the product must not be injected through the pen marks; otherwise a permanent tattooing effect may occur.
For intramuscular injections, the number of injection sites is dependent upon the size of the muscle to be treated and the volume of reconstituted XEOMIN injected.
XEOMIN should be injected carefully when injected at sites close to sensitive structures, such as the carotid artery, lung apices, and esophagus. Before administering XEOMIN, the physician should be familiar with the patient’s anatomy and any anatomic alterations, e.g., due to prior surgical procedures.
Chronic Sialorrhea
Chronic Sialorrhea in Adult Patients:
A sterile needle (e.g., 27-30 gauge (0.30-0.40 mm diameter), 12.5 mm length) should be used for intra-salivary gland administration for the treatment of chronic sialorrhea. The injection site should be close to the center of the gland.
The salivary glands can be located using ultrasound imaging or surface anatomical landmarks [see Dosage and Administration (2.2)].
Chronic Sialorrhea in Pediatric Patients:
A sterile needle (e.g., 27-30 gauge (0.30-0.40 mm diameter), 12.5 mm length) should be used for intra-salivary gland administration for the treatment of chronic sialorrhea. The injection site should be close to the center of the gland.
Ultrasound guidance is recommended for the localization of the involved salivary glands [see Clinical Studies (14.1)].
Upper Limb Spasticity
Upper Limb Spasticity in Adult Patients:
A sterile needle (e.g., 26-gauge (0.45 mm diameter), 37 mm length for superficial muscles; or 22-gauge (0.70 mm diameter), 75 mm length for deeper musculature) should be used in the intramuscular administration in the treatment of upper limb spasticity in adults.
Localization of the involved muscles with electromyographic guidance, nerve stimulation, or ultrasound techniques is recommended.
Upper Limb Spasticity in Pediatric Patients, Excluding Spasticity Caused by Cerebral Palsy:
A sterile needle (e.g., 30-gauge (0.30 mm diameter), 25 mm length for superficial muscles; or 27-gauge (0.40 mm diameter), 37 mm length for deeper musculature) should be used in the intramuscular administration in the treatment of upper limb spasticity in pediatric patients.
Localization of the involved muscles with techniques such as electromyographic guidance, nerve stimulation, or ultrasound is recommended.
Cervical Dystonia
A sterile needle (e.g., 26-gauge (0.45 mm diameter), 37 mm length for superficial muscles; or 22-gauge (0.70 mm diameter), 75 mm length for deeper musculature) should be used in the intramuscular administration in the treatment of cervical dystonia.
Localization of the involved muscles with electromyographic guidance or nerve stimulation techniques may be useful.
Blepharospasm
A sterile needle (e.g., 30-gauge (0.40 mm diameter), 12.5 mm length) should be used in the intramuscular administration in the treatment of blepharospasm.
Glabellar Lines
A sterile needle (e.g., 30-33 gauge (0.3-0.2 mm diameter), 13 mm length) should be used in the intramuscular administration in the treatment of glabellar lines.
2.9 Monitoring to Assess Effectiveness
The median onset of XEOMIN treatment effect occurs within seven days after injection. The typical duration of effect of each treatment is up to 12-16 weeks; however, the duration of effect may vary in individual patients.
10. Overdosage
Excessive doses of XEOMIN may be expected to produce neuromuscular weakness with a variety of symptoms, particularly when treated intramuscularly. Respiratory support may be required where excessive doses cause paralysis of the respiratory muscles. In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis [see Warnings and Precautions (5.1, 5.4)]. Symptomatic treatment may be necessary.
Symptoms of overdose are not likely to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or paralysis.
There is no significant information regarding overdose from clinical studies of XEOMIN.
In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. If you do not receive a response within 30 minutes, please contact the CDC directly at 770-488-7100. More information can be obtained at http://www.cdc.gov/ncidod/srp/drugs/formulary.html#1a.
16.2. Storage and Handling
Unopened vials of XEOMIN should be stored at or below 25°C (77°F). Refrigeration of unopened vials is not required. Do not use after the expiration date on the vial. Reconstituted XEOMIN may be stored in a refrigerator at 2°C to 8°C (36°F to 46°F) for up to 24 hours until time of use [see Dosage and Administration (2.7)].
© All content on this website, including data entry, data processing, decision support tools, "RxReasoner" logo and graphics, is the intellectual property of RxReasoner and is protected by copyright laws. Unauthorized reproduction or distribution of any part of this content without explicit written permission from RxReasoner is strictly prohibited. Any third-party content used on this site is acknowledged and utilized under fair use principles.